Warding off the Blues
Blue light has its pros and cons. Here’s how to help your patients manage it for the best systemic and ocular outcomes.
By Bill Hefner, OD, MEd
Release Date: May 16, 2018
Expiration Date: May 16, 2021
Goal Statement: With growing concern that our vision and health are adversely affected by our inability to unplug, it’s more important than ever to understand the effects of blue light. This article describes what blue light is, where it comes from and its effects on patients’ systemic and ocular health. It also shares ideas on how optometrists can help patients incorporate risk mitigation strategies to ward off its negative effects.
Faculty/Editorial Board: Bill Hefner, OD, MEd
Credit Statement: This course is COPE approved for 2 hours of CE credit. Course ID is 58116-GO. Check with your local state licensing board to see if this counts toward your CE requirement for relicensure.
Disclosure Statements:
Authors: The author has no relationships to disclose.
Editorial staff: Jack Persico, Rebecca Hepp, William Kekevian and Michael Iannucci all have no relationships to disclose.
9th Annual Retina ReportFollow the links below to read other articles from our annual update on retina: Busted Barriers: Triaging Retinal Hemorrhages The Bugs Behind Infectious Retinitis The Larry Alexander Resident Case Report Contest: Cloudy with a Chance of Retinopathy |
There is no arguing that today’s patients are inundated with more screen time than ever before. According to a 2015 survey, 60% of American adults are on their digital devices more than six hours per day, with 28% of those individuals exceeding 10 hours per day.1
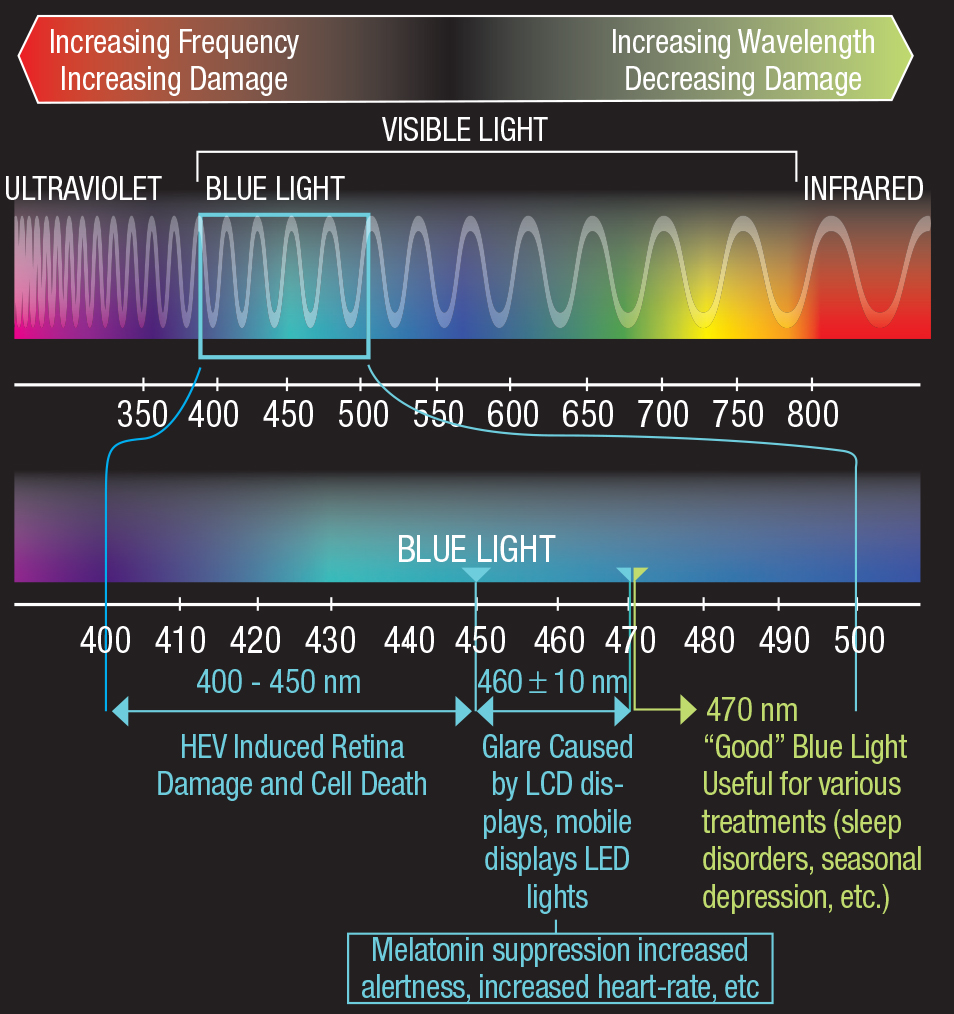
Given the increasing accessibility of cell phones, tablets, computers and more for both education and recreation, we as healthcare providers have to be prepared for a rising tide of significant unintended consequences we don’t yet fully understand.2 In fact, there is growing concern that our vision and health are adversely affected by our inability to unplug.3-5 One particular area of increasing interest is the effects of short wavelength blue light, or high energy visible blue light (HEV). As researchers and vision scientists continue their efforts to identify and quantify the effects of prolonged exposure to HEV emissions from digital devices, including whether or not smart phones, tablets and computers actually give off enough HEV to trigger damage to our visual systems and a decline in our general health, we owe it to our patients to become knowledgable about HEV.
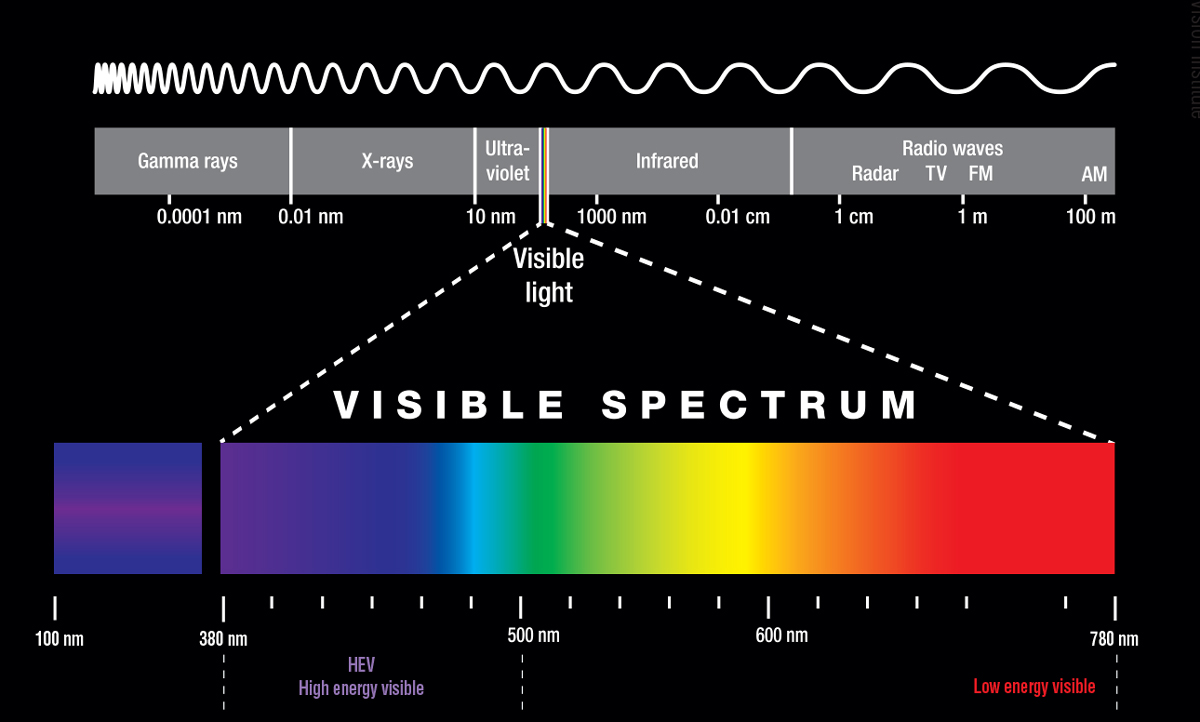 |
| As part of the visible spectrum of light, HEV exposure is inevitable. Image: Adapted with permission from Essilor and Paris |
A Light Primer
Before evaluating the effects of HEV, ODs must first understand what it is and where it comes from. Found in the 380nm to 500nm range, HEV comprises the violet to violet blue end of the light spectrum—and it’s everywhere. And while much of the focus is on HEV emissions from digital devices, we can’t forget about the more energy efficient, higher-output ambient lighting systems that, unlike their incandescent predecessors, pump out significantly more HEV. For example, nearly 35% of cool white light-emitting diode (LED) emissions are in the HEV range, and roughly 26% of compact fluorescent light. In comparison, incandescent bulbs put out less than 12% of their light in the HEV range.6 Artificial light notwithstanding, we should remember that the majority of our HEV exposure comes from the sun, with 25% to 30% of its spectral emissions falling within the HEV range.1
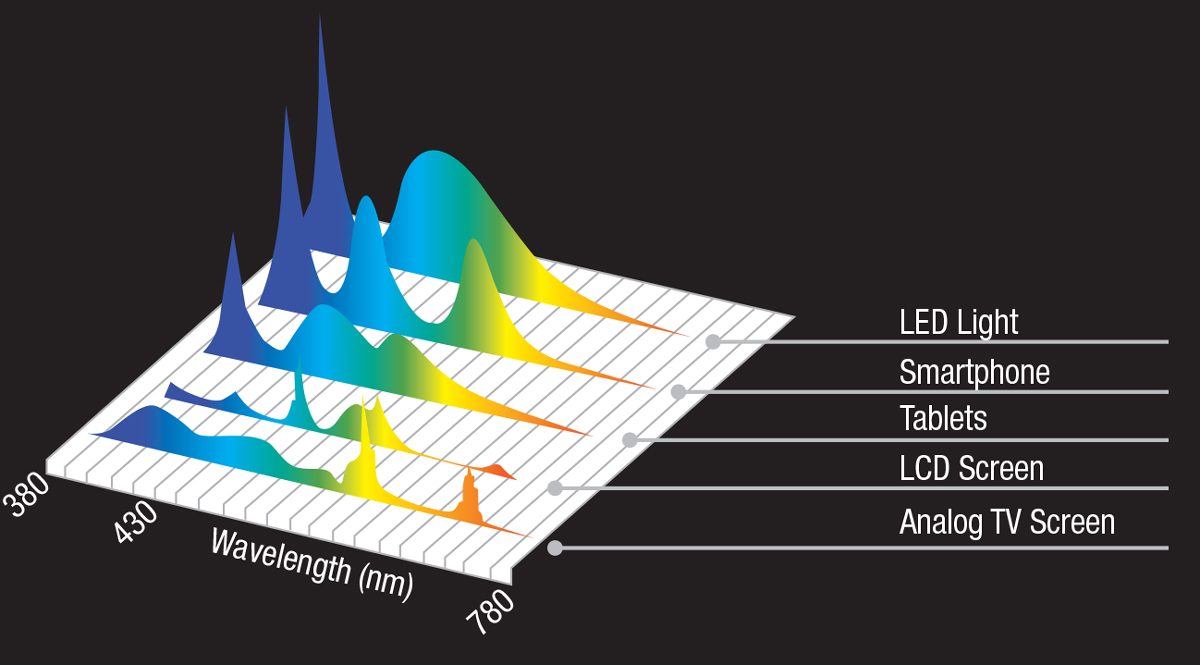 |
| Newer technologies such as LEDs and smartphones emit far more blue light than older technologies such as analog TV screens. Click image to enlarge. Image: Adapted with permission from PFO Global |
While our understanding of the effects of ultraviolet (UV, 380nm and below) and infrared (IR, 780nm and above) light is relatively well developed, we don’t possess a similar grasp of HEV. Luckily, HEV studies continue to yield additional insights into everything from the modulation of the circadian rhythm and improving cognition and memory to HEV’s role in countering myopia progression, as a causative factor in the development of symptoms associated with digital vision syndrome (DVS) and in retinal pigment epithelial (RPE) and photoreceptor cell death.7-13
Based on current research, we can divide the effects of HEV into three broad categories: (1) circadian rhythm modulation with associated impacts on systemic health, (2) ocular effects and (3) medical effects leveraged in the treatment of certain disease processes such as jaundice and dermatological conditions.
This last category is perhaps most well known and understood, as HEV is a mainstay in the treatment of many dermatological conditions such as acne, psoriasis and atopic dermatitis. It also helps to promote wound healing through its antimicrobial and anti-inflammatory side effects.14
What follows is a brief synopsis on the effects of HEV on our patients’ systemic and ocular health and how we can help patients incorporate risk mitigation strategies to ward off the negative effects of blue light while maintaining its benefits.
Table 1. Popular e-Readers and Their Peak Spectral Emissions15 | ||
| Device | Size (in) | Spectral Peak (nm) |
| Book | n/a | 612 |
| iPad | 9.7 | 452 |
| iPhone | 3.5 | 452 |
| Kindle | 6 | 612 |
| Kindle Fire | 7 | 448 |
| Nook Color | 7 | 448 |
Get Into the Rhythm
Many factors affect the human sleep cycle. HEV exposure is a crucial component that has direct relevance to us because of its influence through the visual system and the specialized cells that regulate our circadian rhythm. These intrinsically photosensitive retinal ganglion cells (ipRGCs) have a peak spectral sensitivity between 444nm and 486nm—which, coincidentally enough, is right at the upper end of the HEV spectral range.7 Unlike its photoreceptor siblings, the rods and the cones that undergo hyperpolarization of their cell membranes when stimulated by the wavelength of light corresponding to their chromophores, ipRGCs will depolarize, which ultimately inhibits the release of melatonin from the pineal gland.7
| Kids These Days In a 2014 survey, 85% of parents reported their children are using a digital device more than four hours per day—a number expected to skyrocket with the expansion of “electronic classrooms” (at-home learning) and the incorporation of laptops and tablets into traditional learning environments.2 Educational activities that historically employed chalkboards and overhead projectors are now being supplanted by lesson plans delivered in the asynchronous learning world of BlackBoard, Schoology and similar online learing platforms. While these highlight slick animations and graphics with easy-to-manipulate “plug and play” topical instructions that leverage school-provided tablets and computers, they also expose students to more blue light than ever before. |
Researchers have studied the possible role of ipRGCs on photoentrainment for decades, but with the exponential rise of digital devices in everyday life, interest has spiked. Digital devices aren’t inherently bad; the problem is their LED light sources have higher outputs in the HEV range (roughly 35%) and white light is actually a blue light (peak emission near 450nm) with a yellow phosphor (peak emission around 580nm) that becomes less effective over time.15 In essence, HEV emissions from digital devices that use white LED will actually increase over time.
In 2015, research into the impact of e-readers (e.g., the Apple iPad with a peak wavelength emission of 452nm) on circadian disruption compared with traditional books (peak of 612nm) provided telling results (Table 1). Subjects read from either an e-reader or a book for approximately four hours immediately prior to going to bed, five nights in a row. The authors found the e-reader group had a lag in the onset of sleep by about 10 minutes, a REM sleep period that was shorter by approximately 10 minutes and was subjectively more tired the next day. The most significant finding, however, was the delayed increase of melatonin by nearly two hours.16
 |
| Every light source emits some amount of HEV, and choosing the right lighting can make a big difference in a patient’s daily exposure. Click image to enlarge. Image: Adapted with permission from Essilor and Paris Vision Institute |
While this study could not say whether the findings were due to the light’s wavelength or the intensity of the source itself, a 2017 study confirmed wavelength as the culprit. In this study, subjects were exposed to light sources at either 80lux or 350lux and the light spectrum of 460nm or 620nm for two hours before bed. Each night, researchers collected multiple urine and oral temperature samples and evaluated melatonin levels. While the intensity of light had a negligible effect on sleep quality and melatonin production, the shorter wavelength light had a statistically significant impact on both quality of sleep and melatonin secretion.17
In addition to documenting delayed sleep and increased next-day fatigue, several studies implicate melatonin suppression via HEV-related device exposure in increased levels of insulin resistance, elevated blood pressure, seasonal affective disorder and even certain types of cancers.18-21 One study found subjects exposed to light boxes with a peak wavelength of 468 +/-8nm for 1.5 hours upon waking and 1.5 hours before bed had increased levels of insulin resistance.18 The evening HEV exposure, in particular, led to higher peak glucose production and diminished sleepiness compared with the morning exposure or no exposure to HEV.18
While melatonin plays a vital role in our sleep regulation, blood glucose levels and blood pressure, it’s also a powerful antioxidant with more than just a passing association with certain types of cancer, specifically those related to hormone production such as breast and ovarian. Epidemiological studies demonstrate the association between exposure to light at night (LAN)/decreased melatonin levels and cancer.19 The prospective, longitudinal Nurses’ Health Study II (NHSII), which began in 1989 and now boasts more than 116,000 subjects, has been surveying participants every two years in an effort to gather various health data points as the cohort ages. According to one of their recent releases, women living in areas with higher levels of ambient LAN suffer a higher incidence of breast cancer, particularly in pre-menopausal women with a history of smoking—even after accounting for other risk factors.20 Previous NHSII research also demonstrates creatine-corrected melatonin concentrations were lower in women with >15 pack-years of smoking than in individuals who had never smoked—a significant finding, considering lower melatonin levels are associated with an increased incidence of breast cancer.21 All of this data has led researchers to believe LAN exposure and smoking share similar melatonin-mediated pathways.22
 |
| While many consider blue light harmful, it can have some positive effects, particularly HEV wavelengths above 470nm. For example, the baby in the image below is receiving blue light therapy to treat jaundice. Click images to enlarge. Top image: Adapted with permission from High Performance Optics. Bottom image: Getty Images |
  |
On the Bright Side
HEV-mediated circadian rhythm modulation has some positive attributes as well, perhaps the most encouraging being improved memory and cognition.
Light therapy to treat Alzheimer’s disease is not new, but the applications to other neurodegenerative diseases such as Huntington’s and Parkinson’s are also beginning to show promise.7 In one study, researchers investigated the effects of white LED light on a strain of mice susceptible to developing Alzheimer’s and reached some promising conclusions. In the first of two studies, they implanted a fiber optic probe into the rodents’ hippocampus and flashed white LED light at 40Hz for one hour. The mice had a decrease in the degraded form of the protein tau and a decrease of beta amyloid.9 In the follow-up study, the same strain of mice were placed in a blackout room and exposed to the same white LED light flickering at 40Hz for one hour—with similar results.9 While researchers have yet to determine whether the results are due to the flicker frequency or the HEV emission, the findings continue to advance our understanding of the potential effects of light therapy.
Other studies have evaluated the use of blue light in promoting mental alertness.23 In one investigation, researchers evaluated the effects of daytime and nighttime blue (460nm) and green (555nm) light exposure. Subjects were exposed to either blue light or green light for 6.5 hours in the middle of a 16-hour wake cycle during the biological day. Compared with the green light, exposure to blue light (either at night or during the day) improved auditory reaction times, with electroencephalography readings showing greater activity associated with heightened alertness. The trade-off, however, was that blue light exposure at night increased sleepiness during the day.23
Eyes in the Spotlight
With all the attention on HEV and its effect on our systemic well-being, it’s easy to lose sight of the fact that it also has an impact on our ocular health—issues addressed every day in our clinical care of patients.
Researchers have long known that HEV has a deleterious effect on retinal health.24 It’s been tied to visual changes such as the development of drusen and photoreceptor apoptosis, and DVS.24
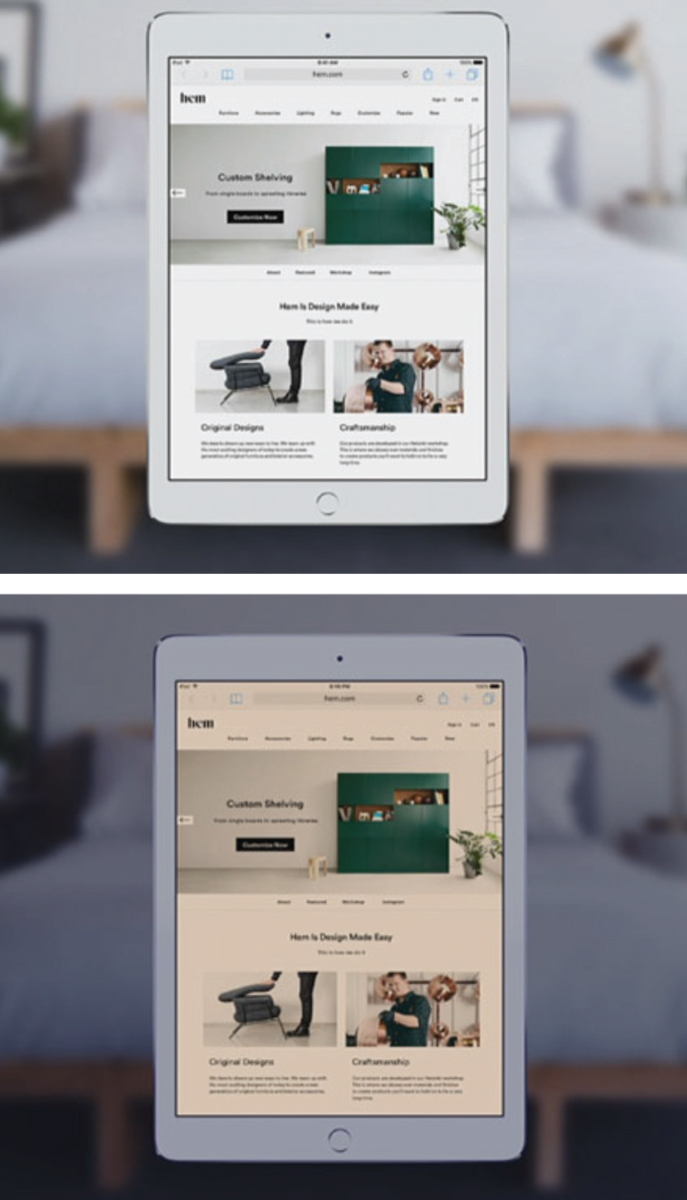 |
| Selective blue light filtering technologies, such as Apple’s Night Shift feature, seen here, can help patients limit HEV exposure at night. Click images to enlarge. Images: Apple |
As blue light enters the eye, it is absorbed by the photoreceptor outer segment, triggering the conversion of the opsin retinal to all-trans-retinal. Subsequent oxidation of the all-trans-retinal leads to the production of reactive oxygen species (ROS) such as singlet oxygen, hydrogen peroxide and other free radicals that accumulate in the photoreceptor outer segment.24 These ROS have an affinity for breaking down cell membranes, causing incomplete phagocytosis of expended photoreceptor outer segments and a build-up of lipofuscin in RPE cells.
Lipofuscin levels are present early in life and gradually increase over time, becoming measurable around age 10 and peaking around age 70.12 However, too much can result in drusenoid changes that can lead to age-related macular degeneration (AMD).12 When lipofuscin and its hydrophobic fluorophore A2E begin amassing in the RPE, the risk of RPE and photoreceptor damage with subsequent death secondary to repeated HEV exposure is at its greatest.
To highlight the significance of HEV in this process, consider the results of this study: after saturating human RPE cells with A2E and exposing them to blue and green light, researchers found RPE apoptosis only occurred in those exposed to the blue light.13 Other researchers using rodent models found exposure to blue LEDs and full-spectrum white LEDs for a period as short as nine days (in 12-hour cycles of light and dark) cause obvious damage to the outer nuclear layer. The researchers attribute the damage to the generation of the ROS during excitation of the photoreceptor cells.25
One missing component in much of this research, however, is the role of the xanthophyll carotenoids lutein and zeaxanthin. These pigments are not only crucial in filtering out short wavelength light before it reaches the photoreceptors and RPE, but also serve as powerful free-radical scavengers.
| Light Among the Stars
|
A fortunate part of the aging process is the natural yellowing of the human lens that increases over time (effectively reducing the amount of blue light reaching the retina); unfortunately, the density of the macular pigments decrease, leaving the eye increasingly vulnerable to HEV’s phototoxic effect. This inverse relationship is profoundly important when considering risk mitigation strategies because it serves as a natural segue into a conversation with your patients about how the loss of macular pigmentation, a family history of AMD and the ever-increasing exposure to HEV (natural or man-made) can fuel the breakdown of the RPE and eventually lead to permanent retinal damage.
Caution should be exercised, however, because in spite of all the available research into the relationship between HEV and AMD, the evidence is still inconclusive. The challenges in establishing a definitive link are wide ranging and include such things as differences in pupil sizes and inter-palpebral fissure width, duration and intensity of the light, the distance from the light source and the actual spectral composition of the light source itself.
Often overshadowed in the HEV-ocular complications research, DVS is another effect of HEV exposure—and one that may affect many more patients than the HEV-AMD relationship. According to a 2015 meta-analysis of the literature, 64% to 90% of computer users experience DVS with symptoms ranging from eye strain and headache/eye ache to blurry vision, diplopia and dry, burning, watering eyes.10 HEV is now implicated in the sequelae associated with DVS because its short wavelength creates a greater propensity for it to scatter as it moves through the ocular tissues, resulting in glare and decreased contrast sensitivity. In addition, this same scatter triggers micro-accommodative changes and, consequently, changes in the phoric posture—a constant “auto-focus” and “auto-depth” that never achieves stability.11
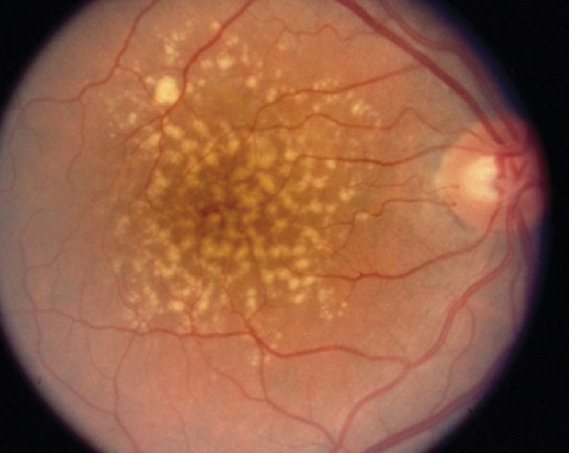 |
| HEV’s known effects on retinal health have led researchers to explore it’s effects on AMD. |
Blue Light Just Right
Rather than completely blocking blue light, patients should take a two-pronged approach to ensure the blue light they are exposed to doesn’t become detrimental to their health. First, patients should eat naturally occurring carotenoids, foods high in omega-3 fatty acids and phytoflavenoids while decreasing risky behaviors such as diets high in saturated and trans fats, smoking and unprotected sun exposure. By changing a diet to consume foods higher in lutein and zeaxanthin, the body becomes better able to form additional macular pigmentation that can protect against macular degeneration due to blue light absorption, reduce photo-oxidative stress and subsequently stabilize RPE cell membranes.26 Second, patients should try to better manage their blue light exposure by incorporating spectacle lenses, smart in-home lighting options and other technologies. While each strategy is equally important, we as optometrists can be particularly helpful with in employing the latter strategy. Some of the blue-filter lens coatings available include: Essilor’s Prevencia (peak absorption between 415nm and 455nm), Kodak’s Total Blue (blocks up to 80% of the HEV between 380nm and 440nm), Hoya’s BlueControl and Zeiss’s BlueProtect (peak absorption between 380nm and 455nm). Gunnar Optiks are specialized computer spectacles designed with peak absorption between 380nm and 470nm. All of these technologies are designed to selectively block harmful HEV, allowing the longer wavelength blue light through and are easy for patients to incorporate into their daily regimens. While they are not the panacea for everything HEV, research shows these coatings decrease harmful effect by between 10.6% and 23.6% while reducing symptoms associated with DVS in roughly 30% of patients.6
Coupling these lens coatings with technologies such as f.lux, Apple’s Night Shift or any blue light-reducing apps for the Android platform will provide patients with even more comprehensive benefits in the areas of phototoxic protection and circadian rhythm stabilization—ultimately reducing the ocular and systemic risks associated with HEV exposure.
HEV exposure is inevitable and has many negative, and a few positive, systemic and ocular ramifications. Each source—the sun, artificial lighting and digital devices—affects us in a different yet predictable manner depending on the distance, intensity, duration and timing of exposure. Our job is to provide patients with recommendations to balance the good and bad effects of HEV, for both their systemic and ocular health. Reducing risky behaviors such as smoking, unprotected sun exposure and poor diet, while increasing healthy behaviors such as dietary intake of naturally occurring carotenoids and phytoflavinoids and incorporating blue light-filtering spectacle lenses and other technologies are all crucial to protecting our patients.
Dr. Hefner spent 20 years in private practice in Topeka, Kan., specializing in pediatrics and family practice optometry before re-joining the faculty at Pacific University College of Optometry in 2017.
He continues to serve in the United States Air Force as the Medical Group Commander for the 190th Air Refueling Wing in Topeka.
Dr. Hefner has provided humanitarian health care in El Salvador, Armenia and Trindad and Tobago. He is a past president of the Kansas Optometric Association, Heart of America Contact Lens Society, and a Fellow of the American Academy of Optometry.
1. Adamopoulos D, Daley M, Hildreth E. Digital eye strain in the USA: Overview by the Vision Council. Points de Vue. International Review of Ophthalmic Optics. 2015;N72. |
