Glaucoma: Lifestyles of the Antioxidant Rich and Famous
Nutrition and other health choices can affect your patients’ risk of disease and progression. Here’s what you need to know to educate them properly.
By Matthew Hochwalt, OD, Heather Spampinato, OD, and Meaghan Horton, OD
Release Date: June 16, 2018
Expiration Date: June 16, 2021
Goal Statement: While more research is needed to better understand nutrition and lifestyle’s role in glaucoma, what we do know suggests some modifications—such as eating foods rich in antioxidants, adding some supplements and even sleeping differently—can be beneficial. This article discusses the current literature on the effects of nutrition and lifestyle on glaucoma risk and progression, so practitioners can be prepared to educate and counsel patients appropriately.
Faculty/Editorial Board: Matthew Hochwalt, OD, Heather Spampinato, OD, and Meaghan Horton, OD
Credit Statement: This course is COPE approved for 2 hours of CE credit. Course ID is 58418-GL. Check with your local state licensing board to see if this counts toward your CE requirement for relicensure.
Disclosure Statements:
Authors: The authors have no relationships to disclose.
Editorial staff: Jack Persico, Rebecca Hepp, William Kekevian and Michael Iannucci all have no relationships to disclose.
Optometrists must arm themselves with the knowledge patients seek so they can answer questions about diet and lifestyle factors, and guide patients toward healthy choices that help to work against glaucomatous progression. Although patient access to health information is ever increasing in the digital age, your recommendations as a healthcare provider likely make a bigger impact on treatment compliance.6
The Theory of Everything Glaucoma
Glaucoma is a complex chronic disease currently understood based on two simplistic models. The vascular model suggests that nerve damage occurs due to reduced or fluctuating blood flow to the optic nerve, while the mechanical model states that intraocular pressure (IOP) compresses and kills the optic nerve neurons.7 Research is also discovering differences at the chemical level of glaucoma patients compared with controls, such as an increase in free radicals (oxidation).8,9 Until we have a better grasp on glaucoma’s mechanism of action, any management with micronutrients through diet or supplementation is still based mostly on theory.
Antioxidants are the focus of most research regarding diet and glaucoma. Oxidation—when an electron is transferred and creates free radicals—is a byproduct of normal cell functions, but can also be produced by stress or environmental toxins.10 Retinal ganglion cell (RGC) mitochondria produce a large amount of free radicals due to their immense energy demands.11 Research suggests free radicals interact with light to directly damage RGCs, and they may also damage the trabecular meshwork, which could compromise aqueous outflow and increase IOP.9 Antioxidants help to stabilize these free radicals by donating electrons to reduce their reactivity.10
 |
| Glaucoma patients with asymmetric cupping/thinning, as seen here, may benefit from some diet modifications such as increased intake of foods rich in antioxidants. Click image to enlarge. |
While increased IOP is currently the main target of glaucoma therapy, research suggests neurodegeneration, including vascular dysregulation, oxidative stress and apoptosis secondary to glutamate toxicity, is also a contributing factor to glaucomatous damage.12-14
Retinal blood vessels’ vascular tone is closely regulated by nitric oxide and endothelin interaction, and patients with normal tension glaucoma (NTG) have an increase in plasma endothelin sensitivity and a decrease in nitric oxide levels.15 On a molecular level, endothelin-1 binds to ETA receptors located on vascular smooth muscle cells, causing an influx of calcium and thus vasoconstriction, decreased blood flow and ischemia, the last of which leads to cellular dysfunction and glutamate retention in intercellular spaces. In glaucoma patients, plasma concentrations of endothelin-1 are increased, reducing blood flow to the optic nerve head and impairing axoplasmic transport.14
Another dietary consideration is glutamate—a major excitatory neurotransmitter in the retina. Excess glutamate results in increased intracellular calcium levels, increased free radical accumulation, oxidative stress, mitochondrial dysregulation and activation of nitric oxide synthase.13,16 Investigators suspect glutamatergic injury is the main cause of RGC death, or apoptosis, in glaucoma.16 When neuronal cells undergo apoptosis secondary to ischemia or circulation disruption, they release additional glutamate, calcium, nitric oxide and free radicals into the extracellular environment, further propagating RGC damage and, ultimately, death.17
Regardless of the exact mechanism, RGC death is the final common pathway of all forms of glaucoma. Therefore, any therapeutic approach to protect these cells—whether medicinal, dietary or lifestyle—can significantly widen the field of glaucoma treatment.18
You Are What You Eat
Science continues to look for specific foods that can help manage glaucoma in conjunction with traditional medical intervention. Unfortunately, the effects of diet on glaucoma are difficult to prove scientifically for several reasons. A typical diet provides more than 25,000 bioactive food constituents and an infinite combination of macro and micronutrients.19 Given this complexity, it is nearly impossible to isolate variables. Added to that, nutrient absorption and use from a certain food can be affected by other foods in the diet. Patient variability is also a challenge, as not all individuals absorb and use nutrients the same way. Thus, a dietary change for one individual will not have the same effect as it might for another individual.20
 |
| Significant RNFL loss in a patient with advanced glaucoma. While the exact mechanism of glaucoma is unknown, the final result is always death of retinal ganglion cells. Click image to enlarge. |
Despite these hurdles, research has uncovered interesting data concerning antioxidant-rich foods and the dietary intake of carbohydrates and essential fats and their effects on IOP and neuroprotection.
Plants. A diet low in fruits and vegetables is associated with a higher prevalence of many chronic systemic and ocular diseases.11 Researchers believe this is due to the high concentrations of bioactive constituents called phytochemicals, a majority of which are antioxidants, in plant-based foods.21 Glaucoma patients in particular show a lower total plasma antioxidant level.8
Studies on the association between a higher intake of fruits and vegetables and decreased odds of glaucoma offer mixed results. One study of older African American women shows a significantly decreased risk of glaucoma with a diet high in fruits and vegetables.22 Another study found specific vegetables such as carrots and leafy green vegetables may be associated with a decreased risk of glaucoma.23 However, the Rotterdam study shows only a decreased risk of glaucoma with dietary vitamin A intake, with all other antioxidants showing no significant benefit.24 They also found a possible increased risk of glaucoma with dietary magnesium intake.24 Other investigators found diets high in carotenoids, vitamin C and vitamin E had no significant correlation with the risk of developing glaucoma.9 Some even found an increased risk of glaucoma with higher consumption of orange juice and spinach.23
A vegetarian diet is an excellent option for incorporating foods high in antioxidants. While fruits and vegetables are phytochemically dense, other plant-based foods show high antioxidant levels as well. Tea, coffee, nuts and seeds contain a significant amount of antioxidants, and some spices and herbs are extremely high in antioxidants as well.21
Nitrates are substances found in high concentrations in green leafy vegetables and may also be protective against glaucomatous damage, especially in individuals with early paracentral visual field loss.25
Carbohydrates. Instead of using antioxidants to neutralize free radicals, limiting carbohydrates can reduce the production of free radicals altogether. Although little research examines the direct relationship of high carbohydrate diets and glaucoma, some investigations show that individuals on a high protein diet have better insulin sensitivity and B-cell function, decreased oxidative stress and inflammatory cytokines compared with those on high carbohydrate diets.26 Researchers also believe mitochondrial dysfunction secondary to oxidative stress may be a risk factor for glaucoma.27
A high glycemic index is also associated with an increase in advanced glycation end products (AGEs) in the retina and brain.28 AGEs are formed from proteins that are nonenzymatically modified by carbohydrates and are associated with cytotoxicity and oxidative stress. These AGEs can induce oxidation and inflammation within the body.29
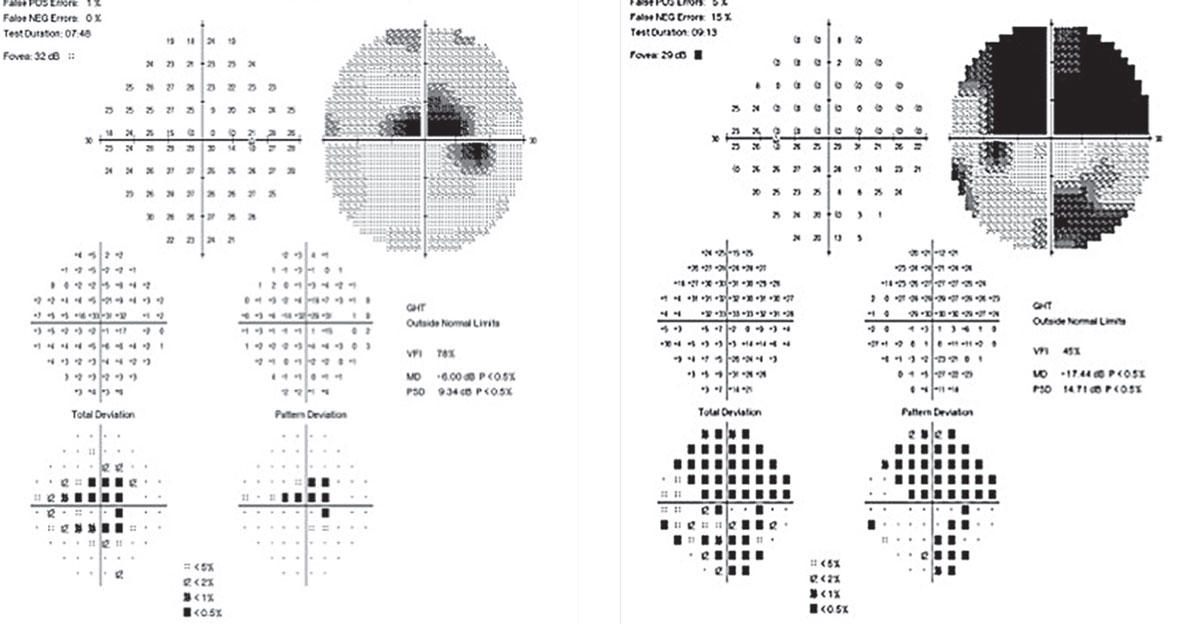 |
| Nitrates found in green leafy vegetables may be beneficial for patients with early paracentral loss to help avoid advanced field loss, as seen here. Click image to enlarge. |
The ketogenic diet, typically consisting of approximately 80% fat, 15% protein and 5% carbohydrates, reduces oxidative stress through the restriction of carbohydrate intake.30-32 Over time, the body’s energy is mainly derived from the oxidation of fatty acids in the mitochondria, producing ketone bodies as the main energy substrate, a process called ketosis.30 This can be neuroprotective in diseases such as Alzheimer’s and Parkinson’s, and is possibly neuroprotective of the RGCs.33,34 One study found that during ketogenic conditions, the brain develops metabolic efficiency by stimulating mitochondrial biogenesis.35 Other investigators found beta-hydroxybutyrate and acetoacetate, compounds produced during metabolism of fatty acids, can also protect neuronal cells from oxidative stress in a rat model.36,37
Fats. The two essential unsaturated fats most frequently studied are omega-3 and omega-6.10 Dietary omega-3 fats, which produce arachidonic acid, are competitive substrates for many enzymes within the eyes. Arachidonic acid and omega-6 derived eicosanoids are precursors of prostaglandin F2-alpha, a well-established ocular hypotensive agent similar to frequently prescribed prostaglandin analog medications.38,39 A diet with a lower omega-3:omega-6 ratio has been shown to reduce the risk of glaucoma in some studies.38,40 Omega-3s, however, have been shown to possibly reduce the risk of glaucoma and have been associated with lower IOP, increased ocular blood flow and improved optic neuroprotection.40,41 One study shows primary open-angle glaucoma (POAG) patients tend to have lower levels of circulating omega-3s.42 Most studies agree that a 1:4 ratio of omega-3 to omega-6 is ideal for an individual’s health, but most western diets range from 1:15 to 1:30.38,43
The Mediterranean diet, high in antioxidants and omega-3s, has long been studied for its many proven health benefits, one of which may be protection for glaucoma patients.44 The diet consists mainly of olive oil, legumes, unrefined cereals, fruits, vegetables, fish and moderate consumption of dairy and wine—creating an omega-3:omega-6 ratio of 1:2.60.45 Others found that individuals with type 2 diabetes on the Mediterranean diet did have a reduced risk of glaucoma.46
Dietary Additions
Patients often ask about supplements touted to have beneficial health effects. These options have some promising research to support their possible positive effects on patients with glaucoma:
Gingko biloba extract (GBE). This contains flavonoids and the terpene lactones ginkgolides and bilobalide, along with several other organic acids. Flavonoids act primarily as free radical scavengers, particularly of nitric oxide, and dilate blood vessels through the release of endothelium-derived relaxing factor and prostacyclin, while also decreasing blood viscosity by antagonizing platelet activating factor.18,47-49 Inhibition of platelet activating factor reduces glutamate excitotoxicity, thereby offering a neuroprotective effect.49 One study demonstrated neuroprotective effects of GBE in RGCs of rats with moderately elevated IOP, primarily through reduction of nitric oxide toxicity.18
Studies evaluating the effect of GBE on ocular blood flow show increases in both peak systolic velocity and end diastolic velocity in the ophthalmic artery of healthy subjects.47 GBE may also increase blood flow through the central retinal and short posterior ciliary arteries in patients with ocular vascular deficiencies such as glaucoma.47 In patients with NTG, GBE can increase peripapillary blood flow, volume and velocity.48 Researchers demonstrated that 40mg of GBE TID for four weeks resulted in a statistically significant improvement in both mean deviation (MD) and pattern standard deviation (PSD) on visual field testing compared with baseline in NTG patients who previously had progressive visual field damage with no significant IOP change.50 However, the visual field improvements were not maintained after discontinuation of GBE treatment, suggesting therapy would have to be long term.
 |
| This patient with advanced POAG has a history of selective laser trabeculoplasty OU and is currently on maximum topical therapy. Dietary and lifestyle changes may be particularly important in this case to help supplement the patient’s medical management. Click image to enlarge. |
While efficacy and safety reports suggest a daily dose of 120mg is acceptable and sufficient for most healthy adults, further studies are needed to better define glaucoma treatment recommendations.14
Flavonoid anthocyanins. These have strong antioxidant properties, inhibit platelet activation and promote collagen synthesis and decreased capillary permeability.17,49 Anthocyanins from Vaccinium myrtillis, or bilberry, can improve best-corrected visual acuity in patients with NTG, likely through effects on ocular blood flow.49 Oral bilberry extract may also provide a neuroprotective effect to RGCs after optic nerve damage through the reduction of oxidative stress and endoplasmic reticulum stress, both of which can signal apoptosis.51
Anthocyanins in black currants can induce endothelin-dependent vessel dilation, resulting in increased blood flow to the inferotemporal rim of the optic nerve head in glaucoma patients.52 Research also shows daily systemic administration of 50mg of black currant anthocyanins can decrease IOP by an additional 0.6mm Hg in glaucoma patients treated with prostaglandins.52
Coenzyme Q10. Also known as CoQ10 or ubiquinone, this is an antioxidant that specifically targets mitochondria and can exhibit neuroprotective activity in a number of neurological disorders, including Parkinson’s and Huntington’s disease.53 It maintains mitochondrial membrane potential and inhibits reactive oxygen species generation, thereby protecting neuronal cells from oxidative stress.16 The level of CoQ10 in the human retina declines by up to 40% with age, suggesting RGCs become more susceptible to glaucomatous neurodegeneration over time.16,53 In one study, dietary supplementation with CoQ10 over the course of six months in glaucomatous mice promoted RGC survival through the inhibition of oxidative stress, glutamate excitotoxicity and apoptosis.16
Another recent study demonstrates a significant neuroprotective effect against RGC loss with topical application of CoQ10 in rats with surgically induced ocular hypertension.53 After three weeks of once-daily application, the number of apoptotic RGCs in the rats was significantly reduced without any effect on IOP.53
Magnesium. This supplement works to inhibit intracellular calcium influx and glutamate in the retina, thereby reducing vascular dysfunction, oxidative stress and RGC apoptosis.54,55 Magnesium deficiency has been associated with retinal pigment epithelium necrosis and myelination disorders of the optic nerve in rats, as well as pigmentary retinal degenerations such as retinitis pigmentosa in humans.55 Magnesium supplementation is relatively safe compared with prescription calcium channel blockers, which have been known to cause hypotension, bradycardia and decreased cardiac output.54,55
In one study, researchers evaluated the effect of oral magnesium on visual field and ocular blood flow in normotensive glaucoma.54 Patients received 300mg of oral magnesium citrate in suspension for one month. Within that time, patients had a statistically significant improvement in both MD and PSD on visual fields compared with the control group.54 Another study showed that 121.5mg of magnesium BID for one month improved peripheral circulation as measured by blood flow velocity and number of capillaries.56
 |
| This glaucoma patient has significant inferior notching. Click image to enlarge. |
Melatonin. This antioxidant acts as a scavenger of light-induced free radicals in the retina, protecting photoreceptor outer segment membranes.15,57 Retinal melatonin levels are regulated by the interaction between the circadian clock and light exposure, rapidly rising during dark and decreasing after light exposure.16 Evidence suggests neuroprotective benefits of melatonin through the reduction of nitric oxide and subsequent increase in the uptake of glutamate from the retina.14,58
Hormone replacement therapy. Females have a lower incidence of POAG compared with males up until the age of 80, which has led researchers to investigate the possible role hormones play in the pathogenesis of glaucoma.59 Studies show that estrogen both reduces RGC loss and decreases IOP in women who undergo hormone replacement therapy.60
While the exact mechanism through which estrogen provides a neuroprotective effect in glaucoma remains unknown, a few hypotheses exist. One is that estrogen activates the growth of collagen and increases the elasticity of various ocular tissues, resulting in decreased IOP. Within the lamina cribrosa, collagen changes lead to a decrease in compression on RGC axons, thereby increasing survival rates of these axons in glaucomatous disease.60 In addition, some studies suggest estrogen causes greater blood flow within retinal arteries, particularly the inferotemporal retinal artery, in postmenopausal women on hormone replacement therapy.61 This effect may be due to upregulation of nitric oxide, which causes vasodilation and the antagonizing effects on endothelium-derived contracting factor, which leads to vasoconstriction.61 Researchers also observed increased neuroretinal rim volume, mean retinal nerve fiber layer (RNFL) thickness and RNFL cross-sectional area, especially in the inferotemporal region of the optic nerve head.61
Get Your Life Together
Several lifestyle habits and environment factors can affect IOP.62-65
Sleep position. Research shows IOP is higher when sleeping in the supine position compared with other sleep positions; sleeping with the head elevated 20 to 30 degrees may lessen the effect of the supine position.63,65-67 A recent study of normal tension and high tension glaucoma patients with asymmetric visual field loss found that of those patients preferring to sleep on their side, approximately two-thirds had worse field loss on their sleep-dependent side.68 However, another study found worse visual field loss in the non-dependent side eye.69 Other researchers found a small, but significant, increase in IOP for the eye on the sleep-dependent side relative to the non-dependent side.70 Clinical application of these findings is not well defined, but it is reasonable to recommend a slight head elevation and possible avoidance of sleeping on the side of the worse eye when significant asymmetry is present.
 |
| Anthocyanins in black currants may increase blood flow, particularly to the inferotemporal rim of the optic nerve head in glaucoma patients such as this one with glaucomatous thinning predominantly in the inferior and inferotemporal region of the optic nerve head. Click image to enlarge. |
Elevated body mass index (BMI). Associations between BMI and glaucoma are far less consistent than those with stroke, hypertension, coronary artery disease and type 2 diabetes.71 Studies have found elevated IOP is associated with obesity, but others found a decrease in the incidence of glaucoma with obesity.72-76
Smoking. While this lifestyle habit affects almost all organs, insufficient evidence currently exists to link cigarette smoking to POAG.77,78 Small case-controlled studies led to mixed results, and both large population studies and further evaluation of observational studies by meta-analysis show no association between cigarette smoking and POAG.79-83
Some early studies of cigarette smoking and IOP found a transient but significant increase in IOP following inhalation.84,85 However, a more recent study in young healthy smokers found no significant increase in IOP immediately after smoking.86 The Blue Mountain Eye Study found a 0.26mm Hg higher IOP in chronic smokers vs. non-smokers.87 Similar results were found in a large UK-based cross-sectional study published in 2016 with more than 100,000 patients; the authors found a 0.19mm Hg higher IOP in smokers vs. non-smokers.88
A retrospective study of glaucoma progression in a Japanese population found an association between smoking and progression of inferior visual field defects in glaucoma patients.89 Although another study found smoking was associated with faster glaucoma progression, this is an area with a scarcity of research.90
Alcohol. Several studies show a dose-dependent and transient lowering of IOP shortly following consumption of alcohol.90-93 This lowering effect is not dependent on the type of alcohol consumed, lasts for two to five hours and may be from one to several mm Hg.91,92 Consuming large quantities of alcohol, though, may increase IOP through a hypervolemic effect.94 Although alcohol causes a temporary decrease in IOP, large population studies show no association between alcohol consumption and POAG risk.75,79,80 Some studies even show an inverse relation in glaucoma risk and alcohol consumption.95,96 Even though there may be some health benefits to moderate alcohol consumption, there is not convincing evidence to suggest a benefit for glaucoma patients.
Exercise. Moderately intense aerobic exercise lowers IOP in individuals with and without glaucoma, though the effect may be more pronounced in glaucomatous eyes.69,97,98 Exercise of increasing intensity shows a larger reduction in IOP.99 The effect of exercise may only last an hour in unconditioned individuals and will also fade in fit individuals within weeks of deconditioning.100-102 Exercise does cause a decrease in blood pressure and possibly ocular perfusion pressure, but whether this impacts glaucoma risk or progression is unknown.103
Some specific forms of exercise that induce positional exertion and Valsalva type maneuvers increase IOP. Weight lifting can cause a transient increase in IOP by several mm Hg that dissipates following completion of the exercise.104 Yoga positions that involve a headstand or that place the eyes below the heart can almost double IOP temporarily, but the IOP returns to baseline a few minutes later.65,94
Although research continues to lag behind patient interest, optometrists must remain up-to-date on the information currently available on the many ways a patient’s diet, nutritional supplementation, exercise and habits can affect their IOP and glaucoma risk. For most patients, broad recommendations for lifestyle modification are not warranted due a lack of compelling evidence linking them to glaucoma. Clinicians can instead focus on patients at substantial risk for progression and those with advanced disease. Regardless of the patient’s disease status, proper education and prudent lifestyle counseling can ensure they remain healthy to ward off glaucomatous progression whenever possible.
Drs. Hochwalt, Spampinato and Horton are staff optometrists at the Cincinnati VA Medical Center and adjunct faculty members at The Ohio State University College of Optometry. Dr. Hochwalt is also an adjunct faculty member at the Illinois College of Optometry.
|
1. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403. 2. Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20:537-44. 3. Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343-50. 4. Ornish D, Brown SE, Scherwitz LW, et al. Can lifestyle changes reverse coronary heart disease. Lancet. 1990;336(8708):129-33. 5. Liu K, Daviglus ML, Loria CM, et al. Healthy lifestyle through young adulthood and presence of low cardiovascular disease risk profile in middle age: The Coronary Artery Risk Development in (Young) Adults (CARDIA) Study. Circulation. 2012;125(8):996-1004. 6. Laugesen J, Hassanein K, Yuan Y. The impact of internet health information on patient compliance: a research model and an empirical study. J Medical Internet Research. 2015;17(6):e143. 7. Kaiser PK, Friedmann NJ, Pineda R. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. Saunders; 2004:446. 8. Mousa A, Kondkar A, Al-Obeidan S, et al. Association of total anitoxidants level with glaucoma type and severity. Saudi Med J. 2015;36(6):671-7. 9. Kang J, Pasquale L, Willett W, et al. Antioxidant intake and primary open-angle glaucoma: a prospective study. Am J Epidemiol. 2003;158:337-46. 10. Reed K. Take the pressure off: Nutrition’s role in glaucoma. Rev Optom. 2009;146(7):50-4. 11. Reed K. Nutrition and glaucoma: Exploring the link. Rev Optom. 2015;152(11):58-63. 12. Mozaffarieh M, Flammer J. New insights in the pathogenesis and treatment of normal tension glaucoma. Curr Opin Pharmacol. 2013;13(1):43-9. 13. Sucher N, Lipton S, Dreyer E. Molecular basis of glutamate toxicity in retinal ganglion cells. Vision Res. 1997;37:3483-93. 14. Mozaffarieh M, Flammer J. Is there more to glaucoma treatment than lowering IOP? Surv Ophthalmol. 2007;52(Suppl 2):S174-9. 15. Doganay S, Evereklioglu C, Turkoz Y, Er H. Decreased nitric oxide production in primary open-angle glaucoma. Eur J Ophthalmol. 2002;12(1):44-8. 16. Lee D, Shim M, Kim K, et al. Coenzyme Q10 inhibits glutamate excitotoxicity and oxidative stress-mediate mitochondrial alteration in a mouse model of glaucoma. Invest Ophthalmol Vis Sci. 2014;55(2):993-1005. 17. Harris A, Gross J, Moore N, et al. The effects of antioxidants on ocular blood flow in patients with glaucoma. Acta Ophthalmol. 2018;96(2):e237-41. 18. Hirooka K, Tokuda M, Miyamoto O, et al. The ginkgo biloba extract (EGb 761) provides a neuroprotective effect on retinal ganglion cells in a rat model of chronic glaucoma. Curr Eye Res. 2004;28(3):153-7. 19. World Cancer Research Fund/American Institute for Cancer Research: Food, Nutrition, Physical Activity and the Prevention of Cancer Research. Washington DC: AICR, 2007. 20. Godber J. Nutrient bioavailability in humans and experimental animals. J Food Quality. 1990;13:21-36. 21. Carlsen M, Halvorsen B, Holte K, et al. The total antioxidant content of more than 3100 foods, beverages, spices, herbs and supplements used worldwide. Nutrition J. 2010;9:3. 22. Gianconi J, Yu F, Stone K, et al. The association of consumption of fruits/vegetables with decreased risk of glaucoma among older African-American women in the study of osteoporotic fractures. Am J Ophthalmol. 2012;154(4):635-44. 23. Coleman A, Stone K, Kodjebacheva G, et al. Glaucoma risk and the consumption of fruits and vegetables among older women in the study of osteoporotic fractures. Am J Ophthalmol. 2008;145(6):1081-9. 24. Ramdas W, Wolfs R, Kiefte-de Jong J, et al. Nutrient intake and risk of open-angle glaucoma: the Rotterdam study. Eur J Epidemiol. 2012;27:385-93. 25. Kange J, Willett W, Rosner B, et al. Association of dietary nitrate intake with primary open-angle glaucoma: A prospective analysis from the nurses’ health study and health professionals follow-up study. JAMA Ophthalmol. 2016;134(3):294-303. 26. Kitabshi A, McDaniel K, Wan J, et al. Effects of high-protein versus high-carbohydrate diets on markers of B-cell function, oxidative stress, lipid peroxidation, proinflammatory cytokines, and adipokines in obese, premenopausal women without diabetes. Diabetes Care. 2013;36:1919-25. 27. Abu-Amero K, Morales J, Bosley T. Mitochondrial abnormalities in patients with primary open-angle glaucoma. Invest Ophthalmol Vis Sci. 2006;47(6):2533-41. 28. Uchiki T, Weikel K, Jiao W, et al. Glycation-altered proteolysis as a pathobiologic mechanism that links dietary glycemic index, aging, and age-related disease (in nondiabetics). Aging Cell. 2012;11:1-12. 29. Tessier F, Obrenovich M, Monnier V. Structure and mechanism of formation of hman lens fluorophore LM-1. Relationship to vesperlysine A and the advanced Maillard reaction in aging, diabetes, and cataractogenesis. J Biol Chem. 1999;274:20796-804. 30. Feeman J, Veggiotti P, Lanzi G, et al. The ketogenic diet: from molecular mechanisms to clinical effects. Epilepsy Res. 2006;68(2):145-80. 31. Rogovik A, Goldman R. Ketogenic diet for treatment of epilepsy. Can Fam Phys. 2010;56:540-2. 32. Freeman J, Freeman J, Kelly M. The ketogenic diet: a treatment for epilepsy. 3rd ed. New York, NY: Demos Health; 2000. 33. Van der Auwera I, Wera S, Van Leuven F, et al. A ketogenic diet reduces amyloid beta 40 and 42 in a mouse model of Alzheimer’s disease. Nutr Metab (lond). 2005 Oct;2:28. 34. Vanitallie T, Nonas C, Di Rocco A, et al. Treatment of Parkinson disease with diet-induced hyperketonemia: a feasibility study. Neurology. 2005;64(4):728-30. 35. Bough K, Wetherington J, Hassel B, et al. Mitochondrial biogenesis in the anticonvulsant mechanism of the ketogenic diet. Ann Neurol. 2006;60(2):223-35. 36. Hartman A, Gasior M, Vining E, et al. The neuropharmacology of the ketogenic diet. Pediatr Neurol. 2007;36:281-92. 37. Zarnowski T, Tulidowicz-Bielak M, Kosior-Jarecka E, et al. A ketogenic diet may offer neuroprotection in glaucoma and mitochondrial diseases of the optic nerve. Med Hypothesis Discov Innov Ophthalmol. 2012;1:45-9. 38. Kang J, Pasquale L, Willett W, et al. Dietary fat consumption and primary open-angle glaucoma. Am J Clin Nutr. 2004;79:755-64. 39. Camras C, Alm A. Initial clinical studies with prostaglandins and their analogues. Surv Ophthalmol. 1997;41(suppl. 2):S61-8. 40. Nguyen C, Bui B, Sinclair A, et al. Dietary omega 3 fatty acids decrease intraocular pressure with age by increasing aqueous outflow. Invest Ophthalmol Vis Sci. 2007;48:756-62. 41. Renard J, Rouland J, Bron A, et al. Nutritional, lifestyle and environmental factors in ocular hypertension and primary open-angle glaucoma: an exploratory case-control study. Acta Ophthalmol. 2013;91:505-13. 42. Ren H, Maqulike N, Ghebremeskel K, et al. Primary open-angle glaucoma patients have reduced levels of blood docosahexaenoic and eicosapentaenoic acids. Prostaglandins Leokot Essent Fatty Acids. 2006;74:157-63. 43. Simopoulos A. Omega-3 fatty acids in health and disease and in growth and development. Am J Clin Nutr. 1991;54:438-63. 44. Rumawas M, Meigs J, Dwyer J, et al. Mediterranean-style dietary pattern, reduced risk of metabolic syndrome traits, and incidence in the Framingham Offspring cohort. Am J Clin Nutr. 2009;90:1608-14. 45. Ambring A, Johansson M, Axelsen M. Mediterranean-inspired diet lowers the ratio of serum phospholipid n-6 to n-3 fatty acids, the number of leukocytes and platelets, and vascular endothelial growth factor in healthy subjects. Am J Clin Nutr. 2006;83:575-81. 46. Mvitu Muaka M, Longo-Mbenza B, Tuolomba D, et al. Role of Mediterranean diet, tropical vegetables rich in antioxidants, and sunlight exposure in blindness, cataract and glaucoma among African type 2 diabetes. Int J Ophthalmol. 2012;5(2):231-7. 47. Chung H, Harris A, Kristinsson J, et al. Ginkgo biloba extract increases ocular blood flow velocity. J Ocul Pharmacol Ther. 1999;15(3):233-40. 48. Park J, Kwon H, Chung W, et al. Short-term effects of ginkgo biloba extract on peripapillary retinal blood flow in normal tension glaucoma. Korean J Ophthalmol. 2011;25(5):323-8. 49. Shim S, Kim J, Choi C, et al. Gingko biloba and bilberry anthocyanins improve visual function in patients with normal tension glaucoma. J Med Food. 2012;15(9):818-23. 50. Quaranta L, Betteli S, Uva M, et al. Effect of gingko biloba extract on preexisting visual field damage in normal tension glaucoma. Ophthalmology. 2003;110(2):359-62. 51. Nakamura O, Moritoh S, Sato K, et al. Bilberry extract administration prevents retinal ganglion cell death in mice via the regulation of chaperone molecules under conditions of endoplasmic reticulum stress. Clin Ophthalmol. 2017;11:1825-34. 52. Ohguro H, Ohguro I, Yagi S. Effects of black currant anthocyanins on intraocular pressure in healthy volunteers and patients with glaucoma. J Ocul Pharmacol Ther. 2013;29(1):61-7. 53. Davis B, Tian K, Pahlitzsch M, et al. Topical coenzyme Q10 demonstrates mitochondrial-mediated neuroprotection in a rodent model of ocular hypertension. Mitochondrion. 2017;36:114-23. 54. Aydin B, Onol M, Hondur A, et al. The effect of oral magnesium therapy on visual field and ocular blood flow in normotensive glaucoma. Eur J Ophthalmol. 2010;20(1):131-5. 55. Ekici F, Korkmaz S, Karaca E, et al. The role of magnesium in the pathogenesis and treatment of glaucoma. International Scholarly Research Notices. 2014;1-7. 56. Gasper AZ, Gasser P, Flammer J. The influence of magnesium on visual field and peripheral vasospasm in glaucoma. Ophthalmologica. 1995;209(1):11-3. 57. Agorastos A, Huber C. The role of melatonin in glaucoma: implications concerning pathophysiological relevance and therapeutic potential. J Pineal Res. 2011;50(1):1-7. 58. Belforte N, Moreno M, de Zavalia N, et al. Melatonin: a novel neuroprotectant for the treatment of glaucoma. J Pineal Res. 2010;48:353-64. 59. Dewundara S, Wiggs J, Sulivan D, et al. Is estrogen a therapeutic target for glaucoma? Semin Ophthalmol. 2016;31(1-2):140-6. 60. Wei X, Cai S, Zhang X, et al. Is low dose of estrogen beneficial for prevention of glaucoma? Med Hypotheses. 2012;79(3):377-80. 61. Deschenes M, Descovich D, Moreau M, et al. Postmenopausal hormone therapy increases retinal blood flow and protects the retinal nerve fiber layer. Invest Ophthalmol Vis Sci. 2010;51(5):2587-600. 62. Mutolo MG, Albanese G, Rusciano D, Pescosolido N. Oral administration of forskolin, homotaurine, carnosine, and folic acid in patients with primary open angle glaucoma: changes in intraocular pressure, pattern electroretinogram amplitude, and foveal sensitivity. J Ocul Pharmacol Ther. 2016;32(3):178-83 63. Lazzaro EC, Mallick A, SinghM, et al. The effect of positional changes on intraocular pressure during sleep in patients with and without glaucoma. J Glaucoma. 2014;23(5):282–7. 64. Hamilton-Maxwell KE, Feeney L. Walking for a short distance at a brisk pace reduces intraocular pressure by a clinically significant amount. J Glaucoma. 2012;21(6):421-5. 65. Baskaran M, Raman K, Ramani KK, et al. Intraocular pressure changes and ocular biometry during Sirsasana (headstand posture) in yoga practitioners. Ophthalmology. 2006;113(8):1327-32. 66. Prata TS, De Moraes CG, Kanadani FN, et al. Posture-induced intraocular pressure changes: considerations regarding body position in glaucoma patients. Surv Ophthalmol. 2010;55(5):445-53. 67. Buys YM, Alasbali T, Jin YP, et al. Effect of sleeping in a head-up position on intraocular pressure in patients with glaucoma. Ophthalmology. 2010;117(7):1348-51. 68. Kim KN, Jeoung JW, Park KH, et al. Relationship between preferred sleeping position and asymmetric visual field loss in open-angle glaucoma patients. Am J Ophthalmol. 2014;157(3):739-45. 69. Kaplowitz K, Blizzard S, Blizzard DJ, et al. Time spent in lateral sleep position and asymmetry in glaucoma. Invest Ophthalmol Vis Sci. 2015;56(6):3869-74. 70. Lee TE, Yoo C, Lin SC, Kim YY. Effect of different head positions in lateral decubitus posture on intraocular pressure in treated patients with open-angle glaucoma. Am J Ophthalmol. 2015;160(5):929-36. 71. Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterol. 2007;132:2087-102. 72. Yoshida M, Ishikawa M, Kokaze A, et al. Association of life-style with intraocular pressure in middleaged and older Japanese residents. Jpn J Ophthalmol. 2003;47:191-8. 73. Klein BE, Klein R, Linton KL. Intraocular pressure in an American community. The Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 1992;33:2224-8. 74. Wu SY, Leske MC. Associations with intraocular pressure in the Barbados Eye Study. Arch Ophthalmol. 1997;115:1572-6. 75. Leske MC, Connell AM, Wu SY, et al. Risk factors for open-angle glaucoma. The Barbados Eye Study. Arch Ophthalmol. 1995;113:918-24. 76. Gasser P, Stumpfig D, Schotzau A, et al. Body mass index in glaucoma. J Glaucoma. 1999;8:8-11. 77. Abraham AG, Condon NG, West Gower E. The new epidemiology of cataract. Ophthalmol Clin North Am. 2006;19:415-25. 78. Thornton J, Edwards R, Mitchell P, et al. Smoking and age-related macular degeneration: a review of association. Eye. 2005;19:935-44. 79. Wilson MR, Hertzmark E, Walker AM, et al. A case-control study of risk factors in open angle glaucoma. Arch Ophthalmol. 1987;105:1066-71. 80. Klein BE, Klein R, Ritter LL. Relationship of drinking alcohol and smoking to prevalence of open angle glaucoma. The Beaver Dam Eye Study. Ophthalmology. 1993;100:1609-13. 81. Stewart WC, Crinkley CMC, Murrell HP. Cigarette-smoking in normal subjects, ocular hypertensive and chronic open-angle glaucoma patients. Am J Ophthalmol. 1994;117:267-8. 82. Leske MC, Warheit-Roberts L, Wu SY. Open-angle glaucoma and ocular hypertension: the Long Island Glaucoma Case-control Study. Ophthalmic Epidemiology. 1997;3:85-96. 83. Quigley HA, West SK, Rodriguez J, et al. The prevalence of glaucoma in a population-based study of Hispanic subjects: Proyecto VER. Arch Ophthalmol. 2001;119(12):1819-26. 84. Shephard RJ, Ponsford E, Basu PK, LaBarre R. Effects of cigarette smoking on intraocular pressure and vision. Br J Ophthalmol. 1978;62(10):682-7. 85. Mehra KS, Roy PN, Khare BB. Tobacco smoking and glaucoma. Ann Ophthalmol. 1976;8(4):462-4. 86. Tamaki Y, Araie M, Nagahara M, et al. The acute effects of cigarette smoking on human optic nerve head and posterior fundus circulation in light smokers. Eye. 2000;14(Pt 1):67-72. 87. Lee AJ, Rochtchina E, Wang JJ, et al. Does smoking affect intraocular pressure? Findings from the Blue Mountains Eye Study. J Glaucoma. 2003;12:209-12. 88. Chan MP, Grossi CM, Khawaja AP, et al. Associations with intraocular pressure in a large cohort. Ophthalmology. 2016;123(4):771-82. 89. Asaoka R, Murata H, Fujino Y, et al. Effects of ocular and systemic factors on the progression of glaucomatous visual field damage in various sectors. Br J Ophthalmol. 2017;101:1071-5. 90. Chiotoroiu SM, Pop de Popa D, tefăniu GI, et al. The importance of alcohol abuse and smoking in the evolution of glaucoma disease. J Med Life. 2013;6:226-9. 91. Peczon J, Grant W. Glaucoma, alcohol, and intraocular pressure. Arch Ophthalmol. 1965;73:495-501. 92. Houle RE, Grant WM. Alcohol, vasopressin, and intraocular pressure. Invest Ophthalmol. 1967;6:145-54. 93. Giurlani BP, Obie LG, Petersen CG, Presley DD. Alcohol and open angle glaucoma-influence on detection, IOP, BP/IOP ratios. J Am Optom Assoc. 1978;49:409-16. 94. Cramer H, Krucoff C, Dobos G. Adverse events associated with yoga: a systematic review of published case reports and case series. PLoS One. 2013;8(10):e75515. 95. Kang JH, Willett WC, Rosner BA, et al. Prospective study of alcohol consumption and the risk of primary open-angle glaucoma. Ophthalmic Epidemiol. 2007;14(3):141-7. 96. Fan BJ, Leung YF, Wang N, et al. Genetic and environmental risk factors for primary open-angle glaucoma. Chin Med J (Engl). 2004;117:706-10. 97. Liang YB, WuY, Li SZ, et al. Physical exercise and intraocular pressure. Chin J Opthalmol. 2011;47(9):854-7. 98. Risner D, Ehrlich R, Kheradiya NS, et al. Effects of exercise on intraocular pressure and ocular blood flow: a review. J Glaucoma. 2009;18(6):429-36. 99. Qureshi IA, Xi XR, Huang YB, Wu XD. Magnitude of decrease in intraocular pressure depends upon intensity of exercise. Korean J Ophthalmol. 1996;10:109-15. 100. Passo MS, Goldberg L, Elliot DL, Van Buskirk EM. Exercise training reduces intraocular pressure among subjects suspected of having glaucoma. Arch Ophthalmol. 1991;109:1096-8. 101. Marcus DF, Krupin T, Podos SM, Becker B. The effect of exercise on intraocular pressure. I. Human beings. Invest Ophthalmol. 1970;9:749-52. 102. McDaniel DR, Tribbey CL, Tobias GS. Effects of moderate exercise on intraocular pressure. Am J Optom Physiol Opt. 1983;60:154-7. 103. Kokkinos P. Physical activity and cardiovascular disease prevention: current recommendations. Angiology. 2008;59(2 Suppl):26S-9S. 104. Vieira GM, Oliveira HB, de Andrade DT, et al. Intraocular pressure variation during weight lifting. Arch Ophthalmol. 2006;124:1251-4. |
