Alternatives to Silicone Hydrogel Contact Lenses
While silicone hydrogel lenses serve many patients well, ponder these five reasons to consider other options.
Goal Statement:
Silicone hydrogel contact lenses are a major technological advance, but many other factors affect successful contact lens wear. This article will analyze a few reasons why you might not consider a silicone hydrogel contact lens as your primary choice in all cases.
Faculty/Editorial Board:
Jason Miller, O.D., Gina Wesley, O.D.
Credit Statement:
This course is COPE-approved for 1 hour of CE credit. COPE ID is 33473-CL. Please check your state licensing board to see if this approval counts toward your CE requirement for relicensure.
Joint-Sponsorship Statement:
This continuing education course is joint-sponsored by the Pennsylvania College of Optometry.
Disclosure Statement:
The authors have no financial relationships to disclose.
 Advances in contact lens
technology over the past 20
years have been tremendous
in terms of ocular health, visual
performance and ease of prescribing
by the eye care professional. Despite
these advances, many factors influence our patients' comfort with
contact lens wear. Fortunately, significant improvements include the
advent of new materials designed to
improve vision and hydration and
increase oxygen permeability—all
to allow lasting comfort. So, is the
newest and most advanced always
"best" for our patients?
Advances in contact lens
technology over the past 20
years have been tremendous
in terms of ocular health, visual
performance and ease of prescribing
by the eye care professional. Despite
these advances, many factors influence our patients' comfort with
contact lens wear. Fortunately, significant improvements include the
advent of new materials designed to
improve vision and hydration and
increase oxygen permeability—all
to allow lasting comfort. So, is the
newest and most advanced always
"best" for our patients?
Silicone hydrogel contact lenses were a major technological advance. The improvement in oxygen permeability was much needed, but many other factors affect successful contact lens wear, such as deposition likelihood, movement and wettability. Oxygen flow is important, but may not tip the scale in ultimate favor for fitting silicone hydrogel lenses 100% of the time. This article will analyze a few reasons why you might not consider a silicone hydrogel contact lens as your primary choice in all cases.
1. Comfort is King
For contact lens wearers, the goal is to maximize comfort. Practitioners must sort through a range of options to determine the optimal treatment protocol that will improve their patient's comfort level.
As practitioners, we must understand that comfort is a very subjective term. If you were to ask patients to rank their comfort on a 10-point scale, those wearing silicone hydrogels may have lower scores. This may be a result of the fact that many silicone hydrogels have a much higher modulus than conventional hydrogel contact lenses. In addition to a possible foreign body sensation due to a stiffer material, this characteristic may result in minor edge lift issues if the material is too loose.
| The Many Benefits of Disposability |
| It is important to actively discuss the new materials and modalities available, along with their improved health benefits. In many instances, hydrogel daily disposable contact lenses may be the best choice. The one-day modality offers patients the convenience of a fresh lens each time, without the hassle of cleaning and keeping track of a replacement schedule. Also, one-day contact lenses are very useful for patients who have had a history of non-compliance, solution or material sensitivity or toxicity. This lens modality may be the best choice for our pediatric and teen population—our often not-so-responsible patient population. Statistically, daily disposable lens wearers have the lowest rate of complications, which opens up the potential to add a significant number of contact lens wearers to your office. These lenses offer many advantages, of which convenience is by far the biggest. In the end, the best lens to use is the one that maximizes their comfort.12-14 |
For patients with these types of complaints, it is important to create a strategic approach to better achieve comfort. Here's how:
- Treat any underlying condition. An underlying ocular health issue may be the root cause of the discomfort. Dry eyes can have a huge impact on the contact lens wearer and the contact lens practice. According to the National Eye Institute's Impact of Dry Eye on Everyday Life (IDEEL) questionnaire, approximately 34% of contact lens wearers discontinue use at least once, most frequently as a result of dry eye symptoms.1,2 This can slowly erode a contact lens practice. A thorough history is the first step in identifying the dry eye patient.
- Focus on contact lens care. It is important to look for ways to modify the care system regimen to optimize comfort. This entails getting a true account of the patient's care routine and making sure that he or she is using the solutions that will most likely improve the wearing experience. If your patient has strayed from prescribed wear and care patterns, take the time to go over proper care techniques.3
- Evaluate the material. A number of contact lens materials and designs can improve the comfort level that a patient is experiencing. Silicone hydrogel lenses, in particular, have been designed to maximize oxygen permeability, but not always maximize comfort. However, recently, there have been significant technological advancements in surface chemistry designed to improve the hydration of second and third generation silicone hydrogels.
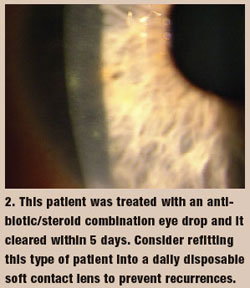
- Evaluate the modality. Always prescribe patients' preferred wearing schedule, while considering their ocular health and compliance. From single-use daily disposable contact lenses to two-week, one-month and the less common, quarterly/yearly replacement schedules, today's contact lens wearers have many options to consider when choosing a lens modality. But ultimately, as the eye care practitioner, you are responsible for selecting a proper contact lens modality and material to ensure lens wear success. All things considered, the lens and lens care system that minimizes patients' chances for an infectious or infiltrative event is the one you should choose. For many patients—particularly those who are non-complaint—daily disposable lenses may be the wisest option (see sidebar). Likewise, astigmatic patients often will be best served with alternative lens options. A significant portion of these patients wear spherical equivalent contact lenses to mask the uncorrected cylinder, but this technique often does not provide optimal vision correction. New introductions of daily disposable options in toric designs will give us yet another opportunity to engage current and potential lens wearers with this convenient modality
2. History of "Corneal Event"
A thorough contact lens fit and the process of individualizing the contact lens wearing experience starts with a thorough history, which includes asking about previous red eyes, corneal ulcers, infectious reactions and inflammatory events. Superior epithelial arcuate lesions (SEALs) are multifactorial, but may be a direct result of mechanical irritation from a stiffer silicone hydrogel material.4 The incidence is increased with silicone hydrogels.5 Patients may not specifically know what happened, but can often describe the situation and how it was treated—so, don't forget to ask!
The increased stiffness of silicone hydrogel lenses may also result in higher numbers of mucin balls. These coalesced mucins are also a result of a mechanical complication of silicone hydrogels, can affect vision and may be transient.6 Patients may complain of visual fluctuations, but upon examination, you may or may not see the mucin balls. Although most patients adapt and the number of mucin balls decreases over time, it can possibly be a longstanding issue.
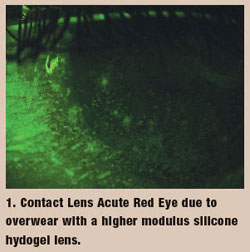
In addition, an unexpected finding with silicone hydrogel lenses has been an increase in infiltrative events. Much research is ongoing in this area, but corneal hypoxia may not play as large a role as previously thought with regard to these events. Dr. Szczotka-Flynn has speculated that the improved physiological profile of the cornea beneath a silicone hydrogel lens may allow for more rapid activation of the immune response against bacterial ligands frequently present on all lens surfaces.7 Patients with a past history of infiltrative events while wearing silicone hydrogel lenses is another reason to consider other contact lens options.
 3. Heavy Depositor
3. Heavy Depositor
Some patients are heavy depositors and have difficulty keeping silicone hydrogel lenses clean due to the increased likelihood of lipid-based deposits. Unlike traditional hydrogel challenges with proteinbased deposition, lipid-based deposits are more transient and may actually slide around on the lens surface, affecting vision and comfort in a dynamic manner.8,9
Traditional enzymatic cleaners may not eliminate these deposits. Although more frequent replacement modalities help to minimize this situation, you will still have some patients who are truly at a disadvantage with their silicone hydrogel lenses after only a few days of wear due to lipid deposits. Additionally, the lipid deposits create more risk of biofilm formation, which may prove very hard to eradicate, and create a higher chance of microbial contamination of lenses and cases.10 What to do? Oftentimes, protein deposition is better managed, or a heavy lipid-depositor may not be as deposit-prone, if fit in a traditional hydrogel lens.
4. Material - Solution Incompatibility Issues
This is not always a reason to walk away from silicone hydrogel contact lenses, but if this becomes a recurrent issue, it may be a reason to change materials and solutions to solve the situation. There is substantial debate surrounding recent studies that implicate solutions and material incompatibility and resultant corneal staining. Despite the ongoing controversy over the details, however, one cannot deny there are possible complications. The more porous nature of silicone hydrogel materials has created an issue of possible solution uptake into the lens matrix. This solution, which was never meant to "wash" the eye during wear time, has been shown to possibly cause loss of corneal integrity, presenting as corneal staining. Research indicates that this staining often does resolve after several hours, and patients may not be at any increased clinical risk of adverse events.11 However, we must consider the possible comfort and visual fluctuation issues that arise from even short-term staining and irritation. Even if a "clinical" finding does not manifest itself, this point is irrelevant to the wearer of said lens and incompatible solution, who experiences a short period of discomfort and non-ideal lens wear every day. Finding these patients is as easy as asking about wear time and comfort/vision throughout the day. Consider lens/ solution combinations, and ask yourself whether silicone hydrogel lenses are truly the best option for these patients.
5. "Tinted" Lenses
This is an easy discussion, as there are no current options for silicone hydrogel tinted, or colored, contact lenses. This may change in the future, but as of now, these patients need to be fit in hydrogel technology. Don't forget to present this option to your patients, as they might not know it's a possibility. Part-time colored lens wear may be something your silicone hydrogel lens wearer may be interested in. Letting them know the technology is somewhat different will set expectations appropriately.
We are fortunate to practice in a time of great innovation within the contact lens arena. However, it's also important to keep in mind the variety of lenses available to us. With the plethora of options out there, mixing some traditional technology with the newest lens options will help keep your contact lens practice healthy and growing.
References
- Pritchard N, Fonn D, Brazeau D. Discontinuation of contact lens wear: a survey. Int Contact Lens Clin. 1999 Nov;26(6):157-62.
- Moss SE, Klein R, Klein BE. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000 Sep;118(9):1264-8.
- Stone R. The importance of compliance: focusing on the key steps. Poster presented, BCLA, May 2007, Manchester, UK.
- Holden BA, Stephenson A, Stretton S, et al. Superior epithelial arcuate lesions with soft contact lens wear. Optom Vis Sci. 2001;78:9-12.
- O'Hare N, Stapleton F, Ndurilath T, et al. Interaction between the contact lens and the ocular surface in the etiology of superior epithelial arcuate lesions. Adv Exp Med Biol. 2002;506:973-80.
- Tan J, Keay L, Jalbert I, et al. Mucin balls with wear of conventional and silicone hydrogel contact lenses. Optom Vis Sci. 2003;80:291-7.
- Jones L, Epstein A, Holden B, Szczotka-Flynn L. The genesis of silicone hydrogels. Contact Lens Spectrum. 2010; 3-15.
- Jones L. Contact lens deposits-patient or material driven? Contact Lens Spectrum. June 2009.
- Gromacki S. Soft contact lens deposition part 1, Contact Lens Spectrum. Feb 2006.
- Wesley G. Biocompatibility and silicone hydrogels. Contact Lens Spectrum. Sept 2009.
- Szczotka-Flynn L. Increased resistance of contact lens related biofilms to antimicrobial activity of soft contact lens care solutions. Cornea. 2009 Sep28;(8):918-26.
- Donshik P, Ehlers W, Anderson L, Suchecki J. Strategies to better engage, educate, and empower patient compliance and safe lens wear: compliance: what we know, what we do not know, and what we need to know. Eye & Contact Lens. 2007;33(6):430–433.
- Stone R. The importance of compliance: Focusing on the key steps. Poster. BCLA. May 2007. Manchester, UK.
- Nixon GJ. A review of contact lens modalities. Available at: www.clspectrum.com/article.aspx?article=&loc=archive\2006\ march\0306032.htm. (Accessed September 2011).
