Advanced Refractive Solutions for Today’s Presbyopic Patient
An overview of the latest refractive surgical options available for presbyopes and strategies to comanage patients.By David Geffen, OD
Release Date:
June 2017
Expiration Date:
June 15, 2018
Goal Statement:
On completion of this educational activity, participants will be better informed about the latest refractive surgery options available in the United States and be able to educate their presbyopic patients on new refractive solutions.
Faculty/Editorial Board:
David Geffen, OD
Credit Statement:
This course is COPE approved for 2 hours of CE credit. COPE ID is 53791-RS. Please check your state licensing board to see if this approval counts toward your CE requirement for relicensure.Joint-Sponsorship Statement:
This continuing education course is joint sponsored by the University of Alabama School of Optometry.Disclosure Statement:
Author Dr. Geffen is a consultant for Alcon, AMO, Annidis, Bausch + Lomb, eyeBrain Medical, Krypton Vision, ReVision Optics, TearLab, TLC Vision and Vmax Vision, and he is an investor in Bruder Healthcare. Editorial staff members Jill Hoffman and Jack Persico have no relationships to disclose.Supported by: An unrestricted educational grant from ReVision Optics.
Presbyopia is on the rise as the population continues to age. An estimated 1.272 billion people worldwide were presbyopic in 2011, up from 1.04 billion in 2005.1,2 By 2020, this number is projected to increase to almost 1.4 billion.2 U.S. Census Bureau figures suggest that 112 million Americans had presbyopia in 2006, with increasing prevalence over the last decade.3
These rising numbers of presbyopes are impacting eye care practices around the country from a clinical and practice standpoint.
For one thing, presbyopic and older patients bring with them a variety of other eye issues, including cataracts, macular degeneration and diabetic retinopathy—translating into busier practices than ever. In addition, the vision care demands of an older population tend to be higher than those of younger patients, based on our experiences at the Gordon Schanzlin New Vision Institute in San Diego.
Amplifying this presbyopic patient growth is the fact that numbers of ophthalmologists entering the field will be relatively flat over the next three years.4,5 The supply of active ophthalmologists is expected to increase by just 2% through 2020, although associated ophthalmologist manpower needs are expected to jump by 28% in the same period of time.4,5 This provides an opportunity for optometrists to fill the gap of routine patient eye care.
LIFESTYLE NEEDS OF THE PRESBYOPIC PATIENT
Today’s presbyopic patients have higher expectations than in the past about maintaining the freedom of movement they have been accustomed to in their daily activities. We are finding that Baby Boomers and Generation Xers are used to active lifestyles and insist on nothing short of exceptional vision to keep up their busy schedules.
Due to the prevalence of digital devices, many individuals—presbyopes included—are looking at digital screens for many hours per day. Among the younger population, a staggering 73% of Millennials (ages 18 to 35) are already reporting symptoms of digital eye strain.6 Among Generation Xers (ages 36 to 51), 65% of adults in their 40s spend more than five hours a day on digital devices with 66% experiencing symptoms of digital eye strain; and among Baby Boomers (ages 52 to 70), 63.9% of adults in their 50s are reporting these symptoms as well.6 This phenomenon may partially explain why we are seeing presbyopic symptoms at younger ages.
Today’s presbyopes also want to maintain a youthful appearance. For example, some of our patients have undergone cosmetic procedures such as Botox and body sculpting. And many already have had refractive procedures with the goal of getting rid of their eyeglasses. However, frequently they are disappointed when we tell them that they may still need to wear readers. Often, the first question I get is: “Can’t I get more LASIK?”
Furthermore, many presbyopes are grappling with the psychological effects of getting older and struggling with their vision, possibly more so than in the past as a result of the ubiquitous presence of digital devices. One study found that presbyopia was associated with worse vision health-related quality of life than emmetropia in younger individuals.7
As such, it is clear that presbyopes face a host of issues when they visit the eye care professional today. As this growing number of patients with their unique vision and refractive needs come to see us, we need to be ready to meet the demand with new and creative solutions.
HALLMARK SYMPTOMS & SIGNS OF PRESBYOPIA
Presbyopia—the inability to focus at near distance due to a refractive problem—occurs naturally in people as they age. As the lens hardens over time, the eye is not able to focus light directly onto the retina. Aging also affects muscle fibers around the lens, making it harder for the eye to focus on close objects, so the lens forces light to concentrate behind the retina, resulting in poor vision for near objects.
As with many eye conditions, the key to uncovering patient problems begins with the optometrist asking the right questions. Early presbyopia symptoms characteristically will include the following presentations, so plan to ask patients about these indications:8
- Blurred vision and the inability to see fine details at near distances due to decreased amplitude of accommodation.
- Ocular discomfort or eyestrain after prolonged near work due to the tromboning effect of images moving in and out of focus.
- Minor headaches, squinting, fatigue or drowsiness from near work related to contraction of the orbicularis muscle or portions of the occipitofrontalis muscle. As a result of the physical effort needed for accommodation to maintain clear near vision, patients can also become frustrated and tense.
- Diplopia associated with increased exophoria and decreased positive fusional vergence amplitude.
- Need for brighter reading light to force pupillary constriction for greater depth of focus.
LIMITATIONS OF EXISTING DISTANCE CORRECTION
With that said, presbyopic distance correction—including bifocal, trifocal and progressive spectacles; and multifocal and monovision contact lenses—is limited by various factors.
To start with, though customized progressive spectacles or presbyopic contact lenses can provide satisfactory near and distance vision to presbyopes without the potential risks of surgery, they cannot restore the true accommodation process of a younger individual.9
And while monovision correction of presbyopia is associated with vision health-related improvements, life quality measures are still rated worse than those of younger subjects with emmetropia in several areas, according to the findings of a 2003 study.7
From a patient satisfaction perspective, some patients tell us they are unhappy with their existing presbyopic correction because they think their eyeglasses make them look older. Others say they feel restricted by the use of eyeglasses or contact lenses, and seek the freedom they had as emmetropes or with previous refractive surgery. Yet other patients dislike the compromise in their distance acuity with monovision correction.
As a result of many of these complaints, we frequently get inquiries from presbyopic patients about possible surgical techniques to improve their vision.
TRADITIONAL SURGICAL OPTIONS FOR PRESBYOPES: WHERE MONOVISION FALLS SHORT
A number of factors have prevented widespread acceptance of traditional surgical correction for presbyopia.9 These include: the fact that the procedures are more invasive; do not consistently produce high-enough quality vision; have the potential for resulting optical and visual distortions, regression of effects and complications such as corneal ectasia and haze, and anisometropia after monovision correction; and run the risk of impairment to distance vision.9
That being said, conventional surgical procedures to help presbyopes regain near vision include:
LASIK (laser in-situ keratomileusis) and PRK (photorefractive keratectomy). These refractive surgeries to correct myopia, hyperopia and astigmatism have been in existence for nearly 20 years. However, for near correction, monovision (i.e., correcting one eye for emmetropia and the other eye for myopia) has been the primary solution available for these procedures. With monovision, we find that too great of a difference between the eyes can result in eyestrain and visual compromise in our patients.
PresbyLASIK With Modified Monovision. This aspheric modification of the cornea under a flap (i.e., PresbyLASIK in one eye) uses an excimer laser to create a multifocal cornea by inducing higher-order aberrations that increase depth of focus.10 The procedure may require the patient to continue wearing reading glasses, though to a lesser extent. We have found the most common complaint associated with modified monovision is slight distance blur. This is because the PresbyLASIK eye is corrected to be slightly myopic so patients have better near vision. At our practice, we have not found PresbyLASIK or PRK to be reliable solutions for our patients and rarely recommend them today.
Multifocal LASIK. This procedure corrects presbyopia by using an excimer laser to reshape the cornea into different zones for near, intermediate and distance vision. An individual’s brain selects the given zone that will yield the sharpest vision, depending on the distance of the perceived object. In each zone, light is refracted differently, similar to how multifocal contact lenses correct presbyopia, to restore good vision at all distances. Multifocal LASIK can be performed bilaterally or for modified monovision correction.
EVOLVING SURGICAL PROCEDURES FOR PRESBYOPES: IOLS GAIN TRACTION
Multifocal or accommodating IOL implantation can be a positive alternative for older presbyopes and higher hyperopes. However, many practitioners consider IOLs too invasive for individuals in their mid-40s to early 50s with a healthy crystalline lens, so, generally, we only recommend them for patients over 55 years of age—leaving a large group of presbyopes ineligible.10 In addition, many patients perceive refractive lens exchange to be more invasive than other refractive surgeries, so the audience for these procedures is quite specific.
In spite of these stipulations, IOL adoption has been rapid in the past five years. Available IOLs include:
Refractive IOLs. These IOLs create several focal points with concentric zones of varying optical power.11 Since the aperture of each zone differs, image quality depends on pupil size, and reactivity to light and accommodation.11
Accommodating IOLs. These IOLs fall into two categories: single-optic and dual-optic. Single-optic IOLs alter image focal points through anterior movement of the IOL and changes in the lens architecture.11 To enhance the range of accommodation, dual-optic systems use two lenses: an anterior high plus lens coupled to a posterior minus lens; as the distance between the two lenses changes, optical power is altered.11
Multifocal & Toric Multifocal IOLs. These IOLs are growing in popularity, and new, lower-add multifocal lenses help reduce the size of potential haloes. The IOLs are often better tolerated than older generations with +4D add powers, and we are having good success with these in our practice.
 |
| Figure 1. Click image to enlarge. |
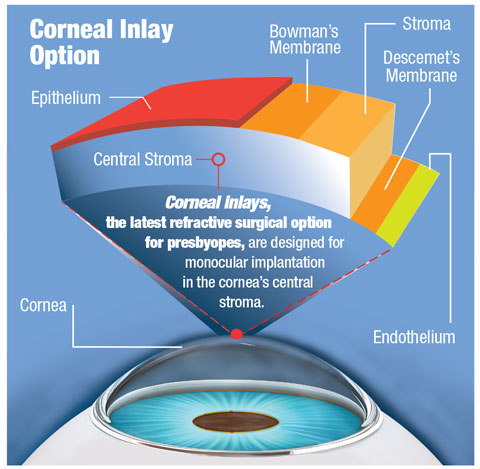
THE LATEST SURGICAL OPTIONS FOR PRESBYOPES: INLAY ADVANCEMENTS
The latest surgical option—corneal inlay implantation—has been available since 2015 in the United States.12 Corneal inlays have several advantages over other refractive procedures. For one thing, the inlays are an additive technology that can be removed in the event of patient dissatisfaction, a complication or onset of other conditions. In addition, the procedures do not remove any tissue, so patients potentially can be candidates for future surgical solutions. And compared to lens surgery, the insertion procedure is less invasive. Plus, depending on the inlay, near correction often remains effective as presbyopia advances.
The three styles of corneal inlays, all designed for monocular implantation in the non-dominant eye, are: corneal reshaping inlays, refractive inlays and small-aperture inlays.
Currently, two corneal inlays are FDA approved, a third is in Phase III trials and a fourth is in development:
 |
| Figure 2. The KAMRA Near Vision Inlay typically is implanted in the non-dominant eye during an outpatient procedure. It is placed within the first few layers of the cornea and centered over the pupil. Photo: Richard Lindstrom, MD |
- KAMRA Near Vision Inlay (AcuFocus). Approved by the FDA in April 2015, this thin (5µm), small-aperture inlay is placed in a pocket in the corneal stroma to increase the patient’s depth of field and improve near vision, but only minimally impact distance vision.13 The opaque ring is 3.8mm wide with a 1.6mm aperture, and the inlay, which houses 8,400 laser holes to facilitate oxygen and nutrient transfer through the cornea, is placed in the non-dominant eye. Similar to a pinhole, near light rays coming through the aperture are focused clearly on the retina. Distance vision is often slightly decreased, typically by two to three lines. If the patient is unhappy with the procedure, the surgeon can remove the inlay, and vision should return to close to the preoperative state.
The KAMRA inlay is indicated for intrastromal corneal implantation to improve near vision by extending the depth of focus in the non-dominant eye of presbyopic patients between the ages of 45 and 60 years of age who have a cycloplegic refractive spherical equivalent of +0.50D to -0.75D with ≤0.75D of refractive cylinder. These patients do not need eyeglasses or contact lenses for clear distance vision, and require near correction of +1.00D to +2.50D of reading add. The ideal patient for this inlay has slight myopia but good distance vision.
The recommended postoperative care regimen includes:
- A broad-spectrum, topical ophthalmic antibiotic QID for a minimum of one week.
- Steroid ophthalmic suspension QID for the first postoperative week, TID for the second week, BID for the third week and QD for the fourth week.
- Preservative-free artificial tears QID for up to one month and continued as needed.
- Punctal plugs may be inserted at any time as needed.
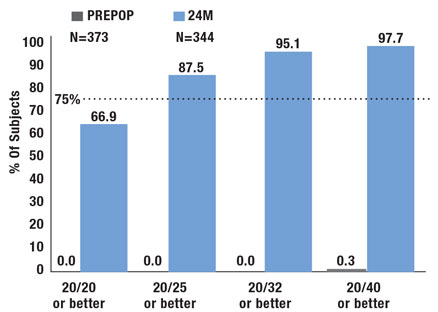
Clinical study results demonstrated an improvement in uncorrected near vision (at 40cm) with the KAMRA inlay.14 The uncorrected intermediate vision (80cm) was slightly improved, while the uncorrected distance vision (6m) in the implanted eyes was slightly decreased.14 The mean changes at 12 months from baseline were: three lines in uncorrected near vision, one line in intermediate vision and half a line in distance vision.14 The effectiveness of the inlay was primarily assessed by monocular uncorrected near vision, and the endpoint target was 75% of subjects with 20/40 or better uncorrected vision in the inlay eye at 12 months post surgery.14
 |
| Figure 3. The Raindrop Near Vision Inlay, indicated for placement in the non-dominant eye to improve near vision of patients, is less than one-tenth of an inch in size and 2mm in diameter. Photo: John Hovanesian, MD |
Preoperatively, none (0/508) of the subjects could see 20/40 or better at near without correction in the eye planned for inlay implantation. At 12 months post surgery, 83.5% (399/478) of subjects had 20/40 or better uncorrected near vision.14 This increased to 87.2% (380/436) at 24 months, 87.1% (363/417) at 36 months and 87.1% (175/201) at 60 months.14 The study successfully met the primary effectiveness criterion of 75%, with the lower 95 CI bound at 79.8% at 12 months post surgery.14
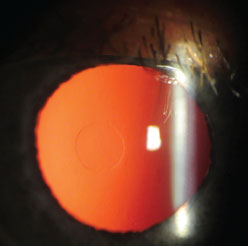
- Raindrop Near Vision Inlay (ReVision Optics). Approved by the FDA in June 2016, this corneal reshaping inlay is made of a hydrogel material and inserted under a flap, similar to LASIK. About 2mm in diameter, 30µm thick and made of approximately 80% water, the inlay is the same refractive index as the cornea. When placed in the cornea, it changes the shape of the central cornea, simulating a multifocal contact lens.
The Raindrop inlay is indicated for use in patients 41 to 65 years old, who have not had cataract surgery, are unable to focus clearly on near objects or small print, and need reading glasses with +1.50D to +2.50D of power. These patients do not need eyeglasses or contact lenses for clear distance vision.
Ideal candidates are those with slight hyperopia (+0.50 to 1.00D) with good distance acuity. Patients cannot have experienced changes in their distance vision within the last year, and they must have healthy eyes. The range of prescription is +1.00D to 0.50D with less than 0.75D of cylinder.
If the patient responds well to a trial contact lens and meets preoperative requirements, the surgeon can go forward with surgery. The inlay is implanted in the non-dominant eye and should only minimally affect distance acuity. If the patient is unhappy or other complications occur, the implant can be removed, and the cornea should return to its preoperative condition.
On average, we have found that patients gain five or more lines of near acuity and about 2.5 lines of intermediate by one week. In studies, at the 24-month visit, 87.5% of patients were 20/25 or better for near, and 76.2% were 20/25 for intermediate.16
Flexivue Microlens (Presbia). Currently in Phase III FDA trials, this hydrophilic acrylic, variable-power inlay has a 3mm diameter, 0.015mm/15µm edge thickness and a plano central zone with increasing rings of higher power. Functioning similar to a multifocal contact lens, the inlay comes in a range of powers. It is inserted under a flap or in a pocket in the non-dominant eye, and the surgeon can remove the lens and replace it with a higher power inlay as the patient becomes more presbyopic. The inlay is offered in powers ranging from +1.5D to +3.5D, in 0.25D increments.
Figure 4. The Flexivue Microlens is placed in a pocket created in the stroma with the aid of a proprietary insertion tool. The pocket self-seals and holds the lens in place at the center of the patient’s visual axis. Photo: Richard Lindstrom, MD
Study results found that 12 months after implantation, uncorrected near visual acuity reportedly was 20/32 or better in 75% of operated eyes, whereas the mean uncorrected distance visual acuity of operated eyes statistically signifcantly decreased from 0.06 ± 0.09 logMAR (20/20).17 Overall, higher-order aberrations increased, and contrast sensitivity decreased in the operated eye. No tissue alterations were found on corneal confocal microscopy, and no intra- or postoperative complications occurred.17 Researchers concluded that the inlay appeared to be an effective way to address the corneal compensation of presbyopia in emmetropic presbyopes between the ages of 45 and 60.17
Overall, higher-order aberrations increased, and contrast sensitivity decreased in the operated eye. No tissue alterations were found on corneal confocal microscopy, and no intra- or postoperative complications occurred.17 Researchers concluded that the inlay appeared to be an effective way to address the corneal compensation of presbyopia in emmetropic presbyopes between the ages of 45 and 60.17
- Icolens (Neoptics). Still in the early stages of development, this hydrophilic copolymer inlay has a 3mm diameter and an edge thickness of less than 15µm (depending on refraction). For presbyopia, the inlay offers powers ranging from +1.5D to +3D (in 0.5D steps). With no power in the center and positive refractive power in the periphery, this inlay’s powers can be exchanged as presbyopia progresses. More information may come on this inlay later.
Preoperative Procedures for Raindrop Near Vision InlayTo help determine whether a patient is a good candidate for the Raindrop Near Vision Inlay, perform a complete eye exam and assess the patient’s general health. Make sure to ask about all medical and eye conditions, and current medications, including over-the-counter products such as vitamins and supplements. Once candidacy is determined and the patient has decided to move forward with the Raindrop Near Vision Inlay:
|
Postoperative Care for Raindrop Near Vision Inlay15
|
Follow-Up Care for Corneal Inlays15,18Follow-up care should be similar for all corneal inlays.
|
CORNEAL INLAY RISKS & WARNINGS
While research is revealing many positive vision outcomes associated with corneal inlays, it is important for eye care professionals to be aware of the possible risks and warnings associated with these new procedures. Some include the following precautions, including:15
- Possibility for new or worsening problems with glare, haloes, blurred or double vision, fluctuation of vision, dryness, foreign body sensation and pain.
- Possible decreased contrast sensitivity.
- Risk of infection, inflammation or both to the front part of the eye.
- Risk of developing a new dry eye condition or worsening of an existing condition.
- Risk of corneal complications.
- Possibility of cataract symptoms worsening or occurring sooner.
- Chance of decreased distance vision in the implanted eye.
- Risk of eye pressure elevation as a result of steroid eye drop usage to suppress inflammation from the procedure.
- Possibility for the need for more surgery to remove the inlay permanently or to exchange the inlay for a new one to treat a complication.
- Possible loss in best-corrected distance vision with eyeglasses or contact lens; in some cases, removal of the inlay will not restore pre-surgery vision.
GROWING INTEREST IN ADVANCED REFRACTION TECHNOLOGIES
According to the 2015 American Society of Cataract and Refractive Surgery Clinical Survey, 70% of member respondents reported that new surgical techniques and technologies such as premium IOLs are topics their patients are most interested in learning about.22 Members also reported that rates of toric and presbyopia-correcting IOL adoption increased at a higher rate than cataract surgery volume during 2014.22
This growing interest in refractive technologies aligns with the fact that today’s presbyopes have higher expectations than those in the past. Today, for example, we are finding that replacing a patient’s cataract with an IOL and then giving the patient eyeglasses for full-time use is no longer acceptable for the average patient. Most presbyopes who come to us expect not to need distance correction after surgery, and many hope not to wear eyeglasses at all.
As well, more patients are doing their own research and are aware of advanced surgical procedures available to them, and they are asking about these options when they come in for visits. As a result, eye care professionals and the profession of optometry as a whole will serve an important role in educating our patients about these new procedures.
We need to be part of the initial conversation to inform our patients about evolving technologies and remain involved in ongoing care plans for patients who decide to go forward with refractive surgery. We find that our patients are interested in learning about advanced surgical options, but very often, they tell us that other eye care professionals never discussed these interventions that could potentially improve their vision outcomes.
Latest Research On Cornea Inlay TechnologyResearch associated with corneal inlay solutions is revealing many positive safety and efficacy outcomes for these vision solutions.19-21 In one prospective, nonrandomized, multicenter FDA Investigational Device Exemption clinical trial that studied the one-year safety and efficacy outcomes of the Raindrop Near Vision Inlay, researchers reported that the inlay provided “significant improvement in near and intermediate visual performance,” with no significant change in binocular distance vision or contrast sensitivity.19
As part of the trial, the non-dominant eyes (n=373) of emmetropic presbyopic subjects were implanted with the inlay at 11 sites; 340 eyes underwent one-year Another study found that the KAMRA inlay was “a viable treatment option” resulting in improved UNVA.20 Researchers in the retrospective chart analysis evaluating six-month postoperative efficacy and safety outcomes in emmetropic presbyopic patients concluded that safety rates were high, while explantation and recentering rates were low.20 They added that increased pocket depth could be associated with better postoperative outcomes.20 In addition, Flexivue Microlens corneal inlay visual outcomes for both near and distance vision were found to be satisfactory in another study, and the inlay did not appear to have significant effects on biometry or IOL power calculations.21 |
APPROACHING THE PRESBYOPIC PATIENT ABOUT REFRACTIVE SURGERY OPTIONS
Eye care professionals owe it to their patients to proactively talk about all available solutions for vision correction. Nothing is worse than running into a patient at the store and finding out that the individual had a surgical procedure that we didn’t know about. Often, when we ask these patients why they didn’t consult with us first, they say we never brought up the topic of surgery so they didn’t think we were knowledgeable in this area.
To avoid this unfortunate scenario, during your summary remarks with presbyopic patients, make sure that you mention new refractive surgical options such as advanced corneal inlay procedures, and why the patient may or may not be a candidate.
To intelligently communicate this information to patients, it is essential that you continue to learn about these advancing technologies. It is also imperative that you maintain good relationships with referring cataract surgeons and stay up-to-date on what procedures surgeons are recommending for your patients. You don’t want your patients to think you aren’t educated on this information and so seek it out on their own. Worse yet, you don’t want to miss the opportunity to comanage your patients, and provide them with preoperative and postoperative care.
TALKING POINTS FOR YOUR PRESBYOPIC PATIENTS
When discussing the pros and cons of different procedures with presbyopic patients who may be candidates for refractive surgical options, it is important to maintain a balanced approach. However, if there are specific attributes of one intervention you feel strongly about, don’t hesitate to tell the patient why.
We must provide patients with the fundamentals of each technology, so they can make an educated decision. At the same time, we need to ensure that we are sending our patients to a reputable surgery center that we trust will keep the patients’ best interests in mind.
FUTURE OF REFRACTIVE SURGERY FOR PRESBYOPIC PATIENTS
Advanced refractive surgical solutions for presbyopes are in their infancy at this time, but they increasingly will play a larger role in all of our eye care practices. It is mission critical that we stay informed about these developments and continue to expand our knowledge about available refractive options for presbyopic patients.
Armed with this intelligence, we will be able to convey accurate information to prospective candidates and coordinate care with the cataract surgeon, helping to ensure that we follow these patients before and after surgery, and well into the future.
Assessing Patient Candidates for Refractive Surgery OptionsHere are important considerations when evaluating a presbyopic patient for refractive surgery:15,23
|
Tips for Partnering With the Right Cataract & Refractive SurgeonSelecting the right corneal surgery partner is not always an easy decision, and your choice should be based on a variety of factors. Don’t make the mistake of collaborating with a surgeon just because their comanagement fee is higher.
|
| 1. Frick KD, Joy SM, Wilson DA, et al. The Global Burden of Potential Productivity Loss from Uncorrected Presbyopia. Ophthalmology. 2015 Aug;122(8):1706-10. 2. Holden BA, Fricke TR, Ho SM, et al. Global vision impairment due to uncorrected presbyopia. Arch Ophthalmol. 2008 Dec;126(12):1731-9. 3. American Optometric Association. Care of the Patient with Presbyopia. Available at: http://www.aoa.org/documents/optometrists/CPG-17.pdf (last accessed January 31, 2017). 4. U.S. Department of Health and Human Services Health Resources and Services Administration Bureau of Health Professions October 2006. Physician Supply and Demand: Projections to 2020. Available at: https://bhw.hrsa.gov/sites/default/files/bhw/nchwa/projections/physician2020projections.pdf (last accessed March 7, 2017). 5. U.S. Department of Health and Human Services Health Resources and Services Administration Bureau of Health Professions December 2008. The Physician Workforce: Projections and Research into Current Issues Affecting Supply and Demand. Available at: https://bhw.hrsa.gov/sites/default/files/bhw/nchwa/projections/physiciansupplyissues.pdf (last accessed March 7, 2017). 6. The Vision Council: 2016 Digital Eye Strain Report. Eyes Overexposed: The Digital Device Dilemma. Available at: http://www.thevisioncouncil.org/sites/default/files/2416_VC_2016EyeStrain_Report_WEB.pdf (last accessed November 30, 2016). 7. McDonnell PJ, Lee P, Spritzer K, et al. Associations of presbyopia with vision-targeted health-related quality of life. Arch Ophthalmol. 2003 Nov;121(11):1577-81. 8. American Optometric Association. Care of the Patient with Presbyopia. Available at: http://www.aoa.org/documents/optometrists/CPG-17.pdf (last accessed January 31, 2017). 9. Papadopoulos PA, Papadopoulos AP. Current management of presbyopia. Middle East Afr J Ophthalmol. 2014 Jan-Mar;21(1):10-7. 10. Black S, Karpecki P, Brooker E, et al. New surgical options for presbyopia. Rev of Optom. 2015 June;152(6)35-42. 11. Crabb A, Krueger, R. The final cut: Surgical correction of presbyopia. Review of Cornea and Contact Lenses. 2014 Nov;151(8):20-6. 12. FDA approves first-of-its-kind corneal implant to improve near vision in certain patients. Available at: https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm443471.htm (last accessed April 12, 2017). 13. Cole J. A closer look at presbyopia correction. Rev of Optom. 2016 Feb;153(2):54-61. 14. Kamra® inlay professional use information. Available at: https://www.accessdata.fda.gov/cdrh_docs/pdf12/p120023d.pdf (last accessed March 31, 2017). 15. Raindrop Near Vision Inlay Patient Information Brochure. Available at: http://www.revisionoptics.com/wp-content/uploads/2016/08/Patient-Information-Brochure-710-0014-Rev-3-Artwork-FDA-Patient-Information-Brochure-US_To-Print.pdf (last accessed April 4, 2017). 16. Raindrop near vision inlay patient information brochure. Available at: https://www.accessdata.fda.gov/cdrh_docs/pdf15/P150034d.pdf (last accessed March 31, 2017). 17. Limnopoulou AN, Bouzoukis DI, Kymionis GD, et al. Visual outcomes and safety of a refractive corneal inlay for presbyopia using femtosecond laser. J Refract Surg. 2013;29:12-8. 18. Dalton M. Correcting presbyopia: Monovision or corneal inlays? Available at: https://www.eyeworld.org/article-correcting-presbyopia--monovision-or-corneal-inlays- (last accessed April 5, 2017). 19. Whitman J, Dougherty PJ, Parkhurst GD, et al. Treatment of presbyopia in emmetropes using a shape-changing corneal inlay: One-year clinical outcomes. Ophthalmology. 2016 Mar;123(3):466-75. 20. Dexl AK, Jell G, Strohmaier C, et al. Long-term outcomes after monocular corneal inlay implantation for the surgical compensation of presbyopia. J Cataract Refract Surg. 2015 Mar;41(3):566-75. 21. Stojanovic NR, Feingold V, Pallikaris IG, et al. Combined cataract and refractive corneal inlay implantation surgery: Comparison of three techniques. Refract Surg. 2016 May 1;32(5):318-25. 22. ASCRS Clinical Survey 2015. Available at: https://www.eyeworld.org/supplements/ASCRS-Clinical-Survey-2015.pdf (last accessed February 7, 2017). 23. Kojima R, and S. Eiden SB. What corneal shape reveals about corneal health. RCCL. 2016 May;30-35. |